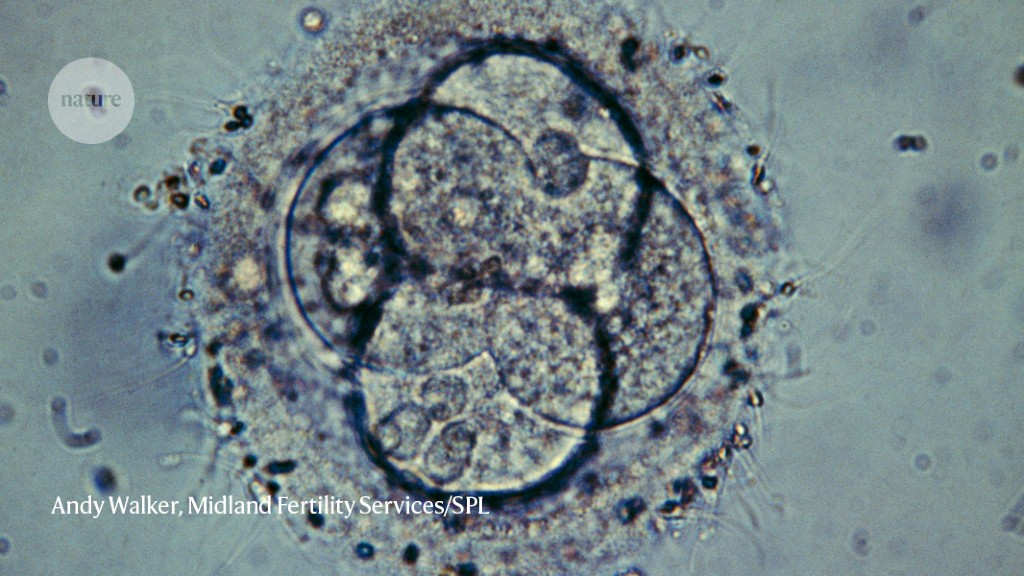
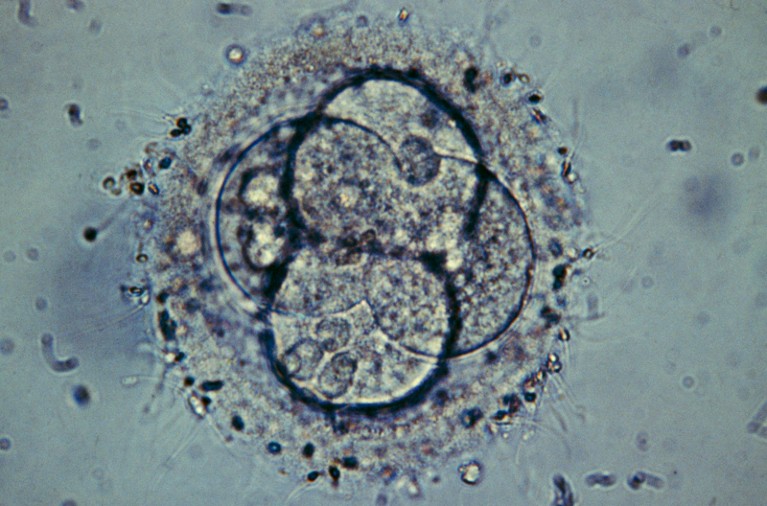
Human embryos could be edited to fix genes that cause genetic diseases. But the science is controversial.Credit: Andy Walker, Midland Fertility Services/Science Photo Library
When researchers gather in London next week for the Third International Summit on Human Genome Editing, they will discuss the latest advances in deploying techniques such as CRISPR–Cas9 to treat genetic diseases, and will look ahead to the possible approval of the first genome-editing therapy later this year.
Despite that tantalizing future, it will be impossible to shake the shadow cast by the previous summit, in 2018. That meeting convened just a day after biophysicist He Jiankui announced that he had edited the genomes of three embryos that developed into living babies. The stunt ultimately earned him three years in prison for breaking China’s laws on medical experiments.
‘CRISPR babies’ are still too risky, says influential panel
Nearly five years later, researchers tell Nature that they do not expect a similar revelation at this year’s summit — if only because He’s experience will dissuade rogue researchers from going public with controversial genome-editing experiments. But that doesn’t mean that such experiments aren’t happening: “I wouldn’t be surprised if there were other children that have been created with CRISPR–Cas9 in the years since 2018,” says Eben Kirksey, a medical anthropologist at the University of Oxford, UK.
Since then, technological aspects of using genome editing to alter human embryos for reproductive purposes have not fundamentally changed, says Robin Lovell-Badge, a reproductive biologist at the Francis Crick Institute in London who is chairing the summit. “It’s still an unsafe technique,” he says, echoing a widespread scientific consensus that genome-editing technology is not ready for use in human embryos.
In the years since He’s revelations, researchers have uncovered further concerns about the use of CRISPR–Cas9 in embryos, including that it can shuffle large segments of chromosomes. This adds to other potential problems with the technique, including the possibility of causing unwanted genetic changes, and of generating a fetus with a mosaic of edited and unedited cells.
Lacking regulation
From a regulatory standpoint, many countries — including the United States — still do not have mechanisms to ensure that edited embryos are not implanted, says Kirksey. In February, China released new guidelines on ethical conduct in biological and medical research. These address the need to inform study participants about potential risks, and provide a detailed description of how ethical review boards should run, says Joy Zhang, a sociologist at the University of Kent in Canterbury, UK. But they still rely on the conventional model of medical research based at hospitals, research institutes and universities, she says. “They ignore the fact that actually, increasingly, private ventures or even individuals can initiate a research project that could be quite damaging and quite cutting edge,” she says. “We need to rethink how we govern.”
CRISPR babies: when will the world be ready?
That includes recognizing that restrictions on how government research funding can be spent might have decreasing influence on researchers’ behaviour, says Zhang. Since his release from prison, He has been courting private investors to back a new project for a gene therapy for Duchenne’s muscular dystrophy. “The bigger question that He Jiankui has raised was not so much creating designer babies per se, but the fact that there’s an increasing number of scientific practices that are outside of conventional scientific institutions,” says Zhang. “How do we track them?”
Furthermore, national regulations do not take into consideration the possible international scope of heritable genome editing, says María de Jesús Medina Arellano, a human-rights lawyer at the National Autonomous University of Mexico in Mexico City. “It’s not that there are no laws. There are many laws,” she says. “We need to change the approach to enforcement. This should be considered an international jurisdiction.”
Affordability concerns
Researchers developing techniques for editing genomes in non-reproductive, or somatic, cells are also wrestling with an upcoming quandary: how to ensure that the therapies are broadly accessible. In 2018, there were very few trials of somatic genome-editing therapies; now there are well over 100, says Lovell-Badge. “Every week, it seems like there’s a new one.”
But prices for existing gene therapies are rocketing, which is making researchers worry that genome-editing therapies will be similarly unaffordable for much of the world. In November, the US Food and Drug Administration approved a gene therapy to treat haemophilia that has been priced at US$3.5 million per treatment. “There’s a lot of hope, but the hope has to be balanced a bit with the way things are going,” says Lovell-Badge.
He Jiankui says he is now working on a a gene therapy for Duchenne’s muscular dystrophy.Credit: Mark Schiefelbein/AP/Shutterstock
Several sessions at the meeting will look at ways to ensure access in low- and middle-income countries — a subject of particular concern this year as regulators in the United States, United Kingdom and European Union weigh up an application from Vertex Pharmaceuticals in Boston, Massachusetts, and CRISPR Therapeutics in Zug, Switzerland, to approve a CRISPR–Cas9 therapy for sickle-cell disease, a genetic condition that mainly affects people of African, Indian or Middle Eastern descent. The treatment could become the first genome-editing therapy to be approved, but researchers are watching anxiously to see how much it will cost.
Over the past year and a half, cardiologist Kiran Musunuru at the University of Pennsylvania in Philadelphia and his colleagues have been developing a genome-editing therapy for the genetic disease phenylketonuria. The team is harnessing variations on the original CRISPR–Cas9 system that, unlike CRISPR–Cas9, do not involve creating double-strand breaks in the DNA. It is hoped that these techniques, called base editing and prime editing, can yield safer genome-editing therapies. But Musunuru says it is important to tackle the affordability question early in development. “I see enormous potential for inequities,” he says.
The radical plan for vaccine equity
Genome-editing technologies must also be tailored to specific DNA sequences. The relative dearth of information on such sequences from individuals of non-European descent could leave regions of the world without access to genome editing therapies that will work for them.
One development that could facilitate access in low- and middle-income countries is the effort to expand vaccine-manufacturing capacity in the global south. Some mRNA vaccines against COVID-19 rely on a lipid nanoparticle to shield the mRNA strand and help it to penetrate cell membranes. It’s possible that genome-editing therapies, which also use snippets of RNA, will involve similar delivery systems, says Musunuru, so could use the same fundamental technology. “If it hadn’t been for the pandemic, we wouldn’t be where we are,” he says. “If you had asked me five years ago if we could do the things we could do now, I would have said, ‘That would be amazing, but no.’”









More News
Chemoproteomic discovery of a covalent allosteric inhibitor of WRN helicase – Nature
Single-cell analysis reveals context-dependent, cell-level selection of mtDNA – Nature
A high-density and high-confinement tokamak plasma regime for fusion energy – Nature