A health worker vaccinates a man in India against COVID-19.Credit: Prakash Singh/AFP/Getty
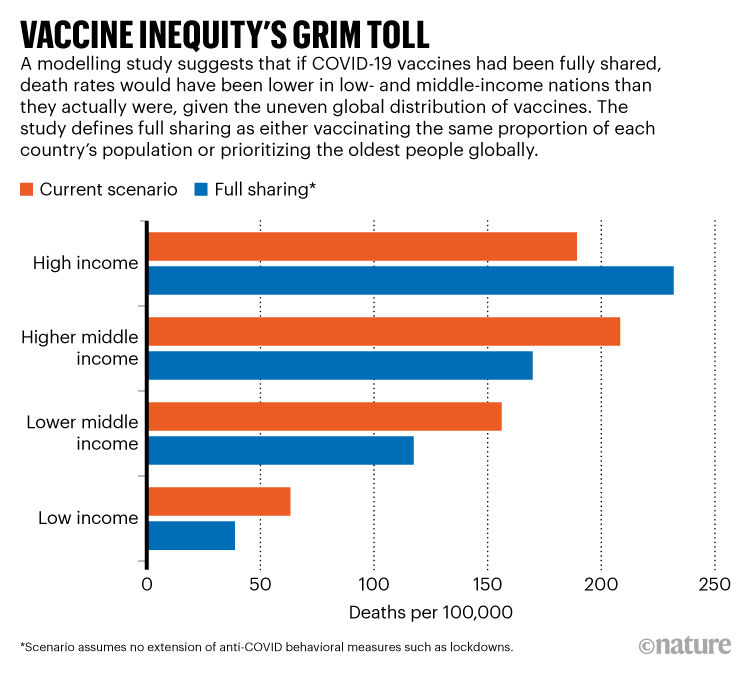
More than one million lives might have been saved if COVID-19 vaccines had been shared more equitably with lower-income countries in 2021, according to mathematical models incorporating data from 152 countries1.
The impact of vaccine sharing would have been even greater if the distribution of more vaccines to poorer countries happened alongside wealthier countries keeping other mitigation measures — such as smaller gatherings and mask wearing — in place for longer. In that case, the models suggest, as many as 3.8 million lives could have been saved.
It has been widely assumed that inequitable vaccine distribution led to unnecessary loss of life. But having an estimate of the size of that loss could aid in planning for future epidemics, says Oliver Watson, an infectious-disease epidemiologist at Imperial College London. “This is another piece of evidence to show how big of an impact pushing for vaccine coverage may have had,” he says. “That’s really important for engaging political will and framing big political decisions.”
Stark gap
By the end of last year, nearly half of the world’s population had received two doses of a COVID-19 vaccine. But those vaccines were not distributed equitably: vaccination rates were 75% in high-income countries, but less than 2% in some low-income countries. Wealthy countries ended the year with vaccine surpluses and plans to vaccinate young children, who are at relatively low risk of serious disease. Meanwhile, many poorer countries still did not have enough supply to vaccinate the people at highest risk of death from COVID-19.
Mathematical epidemiologist Sam Moore and his colleagues at the University of Warwick in Coventry, UK, used data on excess mortality and vaccine availability to model what would have happened if vaccines had been distributed according to need rather than wealth. They considered the impact of vaccination on both SARS-CoV-2 spread and the severity of COVID-19.
The team found that, assuming no other policies that reduced physical contact, more equitable vaccine coverage could have prevented 1.3 million deaths worldwide (see ‘Vaccine inequity’s grim toll’)1. More than twice that many deaths would have been avoided if higher-income countries had also stuck with other measures to reduce transmission. The results were published on 27 October in Nature Medicine.
Source: Ref. 1
The study looked only at vaccine provisions, and did not consider other factors, such as the capacity to store and administer the shots.
The results mesh well with a previous study conducted by Watson and his colleagues, which used a similar modelling technique but with different data. That study found that about 45% of COVID-19 deaths in low-income countries could have been averted if the countries had achieved 20% vaccination coverage by the end of 2021, a target set by the global vaccine-sharing campaign COVAX2.
The pandemic’s true death toll: millions more than official counts
More equitable sharing of vaccines, and a resulting drop in infections, might also have slowed the emergence of fresh SARS-CoV-2 variants, says Moore.
Policymakers could look to studies like these to lay the groundwork for better responses to the next pandemic. Although it might not be realistic to expect countries to give away vaccine supplies before vaccinating their own citizens, governments might be able to find a middle ground, Moore says. “First-world countries might vaccinate everyone over the age of 60 to protect the most vulnerable population, before helping other nations to catch up,” he says. “Even if not equitable, maybe there would be some sort of room for helping other countries once you’ve managed to get your own vaccine in place to some degree.”








More News
Optical clocks at sea – Nature
Publisher Correction: FOXO1 is a master regulator of memory programming in CAR T cells – Nature
India’s 50-year-old Chipko movement is a model for environmental activism