The recent controversial approval of the Alzheimer’s drug aducanumab by the US Food and Drug Administration (FDA) has raised the possibility that the agency could now be more willing to fast-track treatments for a swathe of neurodegenerative diseases — illnesses that have so far thwarted drug developers. But an independent advisory panel fiercely questioned the new drug’s effectiveness, and researchers are divided on whether the potentially smoother approval path that aducanumab has paved will really deliver useful therapies for people with conditions such as amyotrophic lateral sclerosis (ALS), Huntington’s disease and Parkinson’s disease.
Drug developers including Amgen, in Thousand Oaks, California, and Pfizer, based in New York City, have shut down their neuroscience programmes in recent years because of the difficulties of finding successful treatments for brain diseases. So Eric Siemers, a drug development consultant in Zionsville, Indiana, thinks aducanumab’s approval could bring renewed investment and innovation.
On the basis of conversations he has had with investors and clients, he says the tide is already turning. “There’s a lot more interest now in research in neurodegenerative diseases,” says Siemers, who is also chief medical officer of the Alzheimer’s disease company Acumen Pharmaceuticals in Charlottesville, Virginia. Acumen filed paperwork for an initial public offering just days after the approval of aducanumab.
Some advocacy groups are also encouraged, on behalf of desperate patients with few or no therapeutic options. “If the FDA can find a way to be flexible for Alzheimer’s, maybe they can find a way to be flexible for ALS,” says Neil Thakur, chief mission officer at the ALS Association.
But many researchers fear that this regulatory precedent puts false hope above solid clinical science, and harms patients in the process. “Folks who are considering this approach should take a deep breath and a cold shower,” says Fyodor Urnov, scientific director of the Innovative Genomics Institute at the University of California, Berkeley, and a former drug hunter at Sangamo Therapeutics in Brisbane, California.
“I don’t want a future where we have multiple prescribable medicines. I want a future where we have multiple prescribable medicines that work.”
Reading between the lines
Aducanumab — developed by the biotechnology firm Biogen in Cambridge, Massachusetts — followed an unusual route to approval. In March 2019, Biogen halted two phase III trials of the drug candidate after an interim analysis showed that it was unlikely to improve cognition for people with mild Alzheimer’s. But when Biogen re-evaluated the data and found that a subset of people in one of the trials might have benefited, it reversed course; the firm submitted aducanumab for approval in 2020.
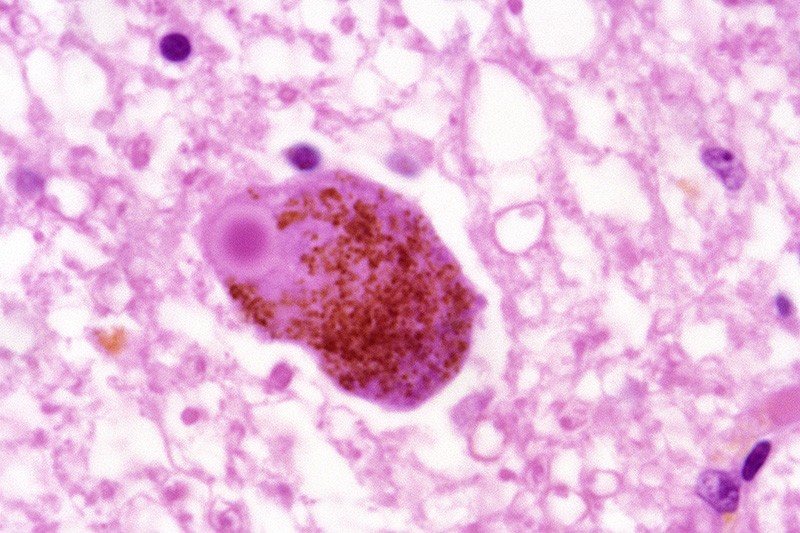
The FDA’s eventual decision to ignore the advice of it advisory committee and approve the drug, it says, was based on aducanumab’s ability to lower levels of amyloid plaques in the brain — protein clumps that some scientists think cause Alzheimer’s.
Instead of granting the drug a standard approval, which is typically reserved for agents that have demonstrated benefit for people in large phase III trials, the FDA opted to use its ‘accelerated approval’ pathway. This is for treatments that are “reasonably likely”, but not certain, to help patients.
The agency has embraced this pathway in cancer, using results from small phase II trials to green-light drugs for narrow sets of patients with late-stage disease. With aducanumab, the agency has shown that it is willing to push the paradigm to a broader set of patients. One reason that decision has attracted criticism is that decreased levels of amyloid plaques are an unvalidated and contentious marker of a drug’s activity.
In large trials of other Alzheimer’s drug candidates, amyloid lowering has not led to cognitive benefits, and this has made it a sticking point for researchers.
Biogen can now sell its US$56,000-per-year drug to 6 million Alzheimer’s patients at all disease stages in the United States. As a condition of the accelerated approval, the firm has until 2030 to report the results of a ‘post marketing’ trial to prove the drug’s cognitive benefit.
Internal memos released last week by the FDA shed some light on the decision. Clinical reviewers argued that aducanumab is likely to provide a cognitive benefit, whereas statistical reviewers said the data did not support approval.
Asked by Nature to elaborate on the implications for Parkinson’s disease, Huntington’s disease and ALS, an FDA spokesperson replied that “the FDA stands ready to work with research communities and drug developers to study more therapies for Alzheimer’s disease and other neurodegenerative disorders”.
Patrizia Cavazzoni, a high-ranking FDA official, has given a nod to aducanumab’s broader impact. “The accelerated approval pathway has been an incredibly useful tool in oncology,” she said in a press meeting. “We believe it serves as a model that we hope can be replicated with neurodegenerative diseases.”
Silver linings?
One neurodegenerative condition whose treatment could benefit from aducanumab’s approval is Parkinson’s disease, which affects an estimated one million people in the United States. Although approved drugs help to alleviate the symptoms of this disease, none of these slows its progression. For Joseph Jankovic, a neurologist at Baylor College of Medicine in Houston, Texas, a more flexible approach to drug development could speed up progress.
The approval of aducanumab “is one of the worst decisions the FDA has ever made,” says Jankovic, who is unconvinced that the drug’s benefits outweigh its risks. But accelerated approval does have value for drugs that offer better hints of efficacy, he argues. “I’m always looking at a glass half full. I hope that this will soften the FDA when they review drugs for other diseases.”
He has his eye on drug candidates that mop up α-synuclein, a protein that builds up in the brains of people with Parkinson’s.
A recent phase II trial of an α-synuclein-targeted antibody called prasinezumab failed to make an overall dent in the symptoms of Parkinson’s disease, Jankovic explains, but it delayed the worsening of people’s tremors, stiffness and slowness of movement. Drug-development partners Roche, based in Basel, Switzerland, and Prothena, in Dublin, have since launched a larger phase II trial to look at the motor-function benefits of the drug candidate.
Results are expected in 2023, at which point this programme could test the FDA’s resolve in relation to neurodegenerative diseases. “In my view, if the phase II study is positive, the FDA should seriously look at the approval of this drug,” says Jankovic, an investigator in trials of the antibody and a consultant to Prothena.
Regulatory goalposts
Huntington’s disease — an inherited neurodegenerative disease that causes involuntary jerking movements and dementia in 30,000 people in the United States — is another one to watch. People with this condition carry a mutant, toxic form of a protein called huntingtin (HTT), so researchers have developed drug candidates to lower its levels.
The most advanced of these had been tominersen, developed by Roche and Ionis Pharmaceuticals, which lowers mutant HTT in the cerebrospinal fluid by 44%. Tominersen entered a phase III trial in 2018. Roche stopped that trial early, in March of this year, after patients worsened on treatment.
HTT-lowering drugs are not yet out of the running, however. Candidates that target other forms of HTT might still slow the disease. And if Roche’s ongoing analysis of the tominersen data identifies any positive trends, the firm will have to decide how to proceed — and whether aducanumab provides a model that it can replicate.
But for Urnov, the failure of tominersen is a prime example of why the FDA should not approve drugs using regulatory goalposts such as amyloid plaques or HTT.
“This is going to harm the prospects for safe, effective, approved medicines for neurodegeneration,” says Urnov. “This is not how our field should be working. This is just not what any of us signed up to do.”








More News
Author Correction: Bitter taste receptor activation by cholesterol and an intracellular tastant – Nature
Audio long read: How does ChatGPT ‘think’? Psychology and neuroscience crack open AI large language models
Ozempic keeps wowing: trial data show benefits for kidney disease