Alan Wang was a healthy man in his twenties when liver cancer started claiming the lives of his relatives. The first to succumb was his uncle Peter, in his mid-fifties. A few years later, it was his uncle Luther. Then his uncle Henry.
In the years that followed, Wang himself experienced two bouts of liver inflammation and was diagnosed with hepatitis B infection, but he didn’t connect his condition to his uncles’ illnesses. It was only later, when he was working in television news and a medical reporter suggested he visit a hepatologist, that the situation become clear. On testing, many of Alan’s family members found that they carried the hepatitis B virus and had probably been infected since birth. As they got older, this infection made them, especially the men, susceptible to hepatocellular carcinoma — the most common type of liver cancer. Alan was at risk, unless he became diligent about treating his infection and monitoring for liver damage.
Liver cancer is the third leading cause of cancer deaths globally — and although rates of death from most types of cancer are decreasing, liver cancer is a notable exception. Rates of fatal hepatocellular carcinoma have risen sharply since the 1980s in the United States and elsewhere, and are projected to increase even further over the next two decades. Excessive alcohol consumption and metabolic disorders both lead to hepatocellular carcinoma, but at the root of most cases are viral infections of the liver. Hepatitis B, in particular, has no cure and is responsible for at least half of all hepatocellular carcinoma worldwide. So preventing cancer in people with hepatitis B could drastically decrease liver cancer cases worldwide — potentially saving around 800,000 lives per year.
When someone’s liver is infected with hepatitis B, damage increases over time, as long as the virus is active. The liver tissue thickens and forms scars (fibrosis), advancing to severe scarring called cirrhosis. In approximately one-third of people with hepatitis B infection, this then progresses to hepatocellular carcinoma, as the viral DNA inserts itself into liver cells, changing their function and allowing tumours to grow.
Researchers and medical professionals cannot yet predict with certainty which people with hepatitis B infection will develop liver cancer. They know it happens more frequently in men, in people infected with certain genetic variants of the virus, in heavy consumers of alcohol, and in those who have been exposed to chemicals called aflatoxins, which can contaminate foods, including peanuts. People with various metabolic disorders are also at higher risk, and studies have identified human genes associated with this viral-led progression to cancer1. However, these risk factors fail to identify everyone who will get hepatocellular carcinoma. People with hepatitis B infection and liver damage should ideally be monitored regularly for evidence of tumours, because survival rates increase if the cancer is caught early.
Interventions with benefits
According to Anna Suk-Fong Lok, a hepatologist at the University of Michigan in Ann Arbor who focuses on viral hepatitis and hepatocellular carcinoma, over the past 40 years, 2 new interventions have given reason for optimism: hepatitis B vaccines that prevent infection, and antiviral therapies that slow liver damage.
In Taiwan, where hepatitis B infection is endemic, all infants have been vaccinated against it since 1984. In the years since, hepatitis-B-associated cancer incidence and deaths have decreased — but only in people born after the vaccine was brought in, Lok says. Children and young adults rarely get hepatocellular carcinoma in the first place, so even a huge decrease in these age groups would barely affect the overall numbers. Nevertheless, Taiwanese viral liver-cancer rates and fatalities are now edging downwards after reaching a peak in the early 2010s.
Antiviral therapies have also helped. These do not eliminate the hepatitis B virus, but do curtail its activity and halt the progression of liver damage. In the United States, they have reduced the occurrence of hepatocellular carcinoma by around 60% in people who receive treatment. The most powerful impact on cancer is seen after five or more years of treatment.
Wang is a success story in this regard: thanks to ongoing antiviral treatment, he currently has an undetectable hepatitis B viral load, and some of his liver damage has reversed. He visits his doctor regularly for monitoring, and no cancer has been detected.
Lok says both interventions will eventually make a difference to liver cancer rates worldwide. “Vaccines will take one generation, 20–30 years, to begin to have an impact, and antiviral therapy will take 5–10 years, even in countries that are early adopters,” she says. “Global impact will take much longer.”
José Manuel Castro Tubío, a geneticist at the University of Santiago de Compostela in Spain, became curious about preventing liver cancer in a different group of people with chronic hepatitis B infection: those who unexpectedly develop hepatocellular carcinoma with minimal liver damage, fast-tracking the normal progression. Tubío says that guidelines for hepatitis B generally do not recommend treatment until liver damage is observed, but it could be time to change that. For some people, he says, “it could be very useful to get the treatment against the virus before the clinical guidelines recommend”.
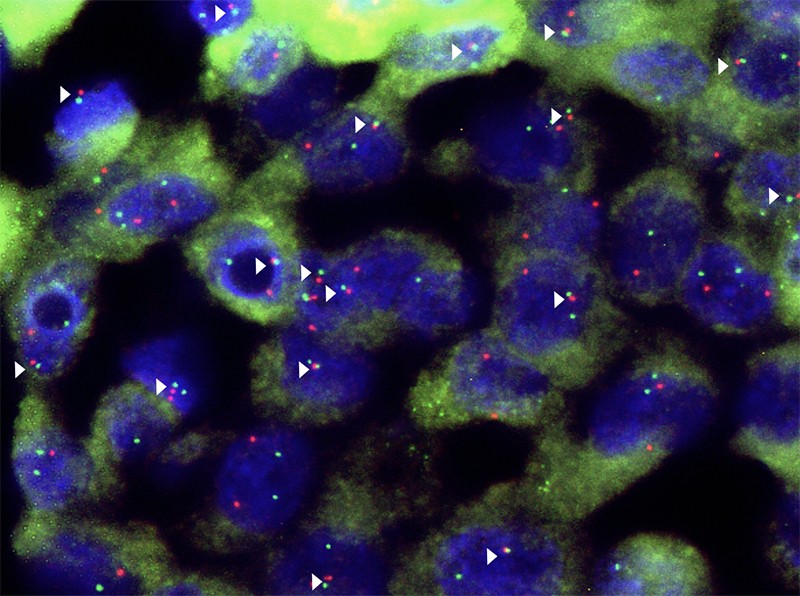
Tubío started with the knowledge that the hepatitis B virus causes cancer by integrating its DNA into human cells. Delving further, his group found2 that the viral break-ins led to chromosome rearrangements, wiping out genes that suppress tumours and allowing cancer cells to proliferate. But the timing was a surprise.
“Some of these events occur as early as 20 years before the diagnosis of the tumour,” says Tubío. “Our results suggest that even in the absence of observable liver damage, there is genetic damage. During this stage, some of the tumours caused by hepatitis B virus start to grow.” Earlier treatment could therefore be essential to finally eliminating liver cancer.
Double disease trouble
Despite these promising strategies, a separate set of chronic health conditions interferes with the prevention of viral-infection-associated liver cancer. Zobair Younossi, a hepatologist at Inova, a health-care provider based in Falls Church, Virginia, says an important reason that liver cancer is still rising dangerously across the globe is the increasing incidence of obesity and related metabolic complications, such as non-alcoholic fatty liver disease (NAFLD) and type 2 diabetes. He explains that, although obesity and fatty liver disease independently put individuals at risk of liver cancer, people who also happen to have hepatitis B infection experience a “double whammy” of liver damage: the virus and the metabolic dysfunction attack the liver in parallel.
Obesity and fatty liver disease are thought to promote cancer through oxidative stress, lipotoxicity — the accumulation of fat-related compounds in non-fatty tissue — and perhaps chemicals released from belly fat that promote inflammation. Some researchers have also proposed that the collection of microbes in the digestive tract — the gut microbiota — could have a role. Jason Behary, a hepatologist at the University of New South Wales in Sydney, Australia, co-led a study3 that analysed gut microbiota in people with NAFLD. He and his colleagues found specific changes in microbial populations and the cocktail of chemicals they produced in people who developed hepatocellular carcinoma. Moreover, extracts from the microbiota had the potential to modulate the body’s immune response, making them strong candidates for driving cancer. Separate studies have found gut microbiota differences in people with hepatitis B infection (without NAFLD) who have developed progressive liver damage or cancer4,5.
Diet direction
Potential gut-microbe-related paths for the development of hepatocellular carcinoma are intriguing, in part because the gut microbiota is strongly influenced by diet, leading researchers to wonder whether dietary modifications could be used to steer away from liver cancer. Elena George, a dietitian and nutrition researcher at Deakin University in Melbourne, Australia, says evidence shows6 that a Mediterranean diet — high in fruit, vegetables and some plant oils — is associated with reduced cancer incidence overall. The limited studies so far conducted specifically on liver cancer also show that similar ‘higher-quality diets’ — rich in fruit and vegetables, and low in sugary drinks and processed meat — reduce risk7.
The lower-quality diets that are so prevalent in the Western world might spell double trouble when hepatitis B infection co-occurs with obesity or metabolic disease. “It is possible that the changes in dietary patterns that are related to the increase in obesity might also be having a direct effect on hepatocellular carcinoma pathogenesis,” George says.
Roughly 300 million people worldwide carry hepatitis B. But the vast majority have no idea they’re at risk, because they are in the dark — either about their hepatitis B status or about how to manage their infection to avoid progression to cirrhosis and cancer.
Younossi emphasizes that a lack of knowledge is the main hurdle. “We need to help educate our patients, our communities, our health-care providers and our policymakers,” he says.
Lok goes further, saying that everyone who did not receive the vaccine as an infant should be screened for hepatitis B. “Only 10–20% of those who are infected have been diagnosed,” she says. “We need to find them through universal testing, not risk-based testing.” Those who test positive could then be started on antiviral treatment. Lok notes that this would flag the individuals who needed to be continually monitored for the development of liver cancer, helping their physicians to catch it earlier so more treatment options are available.
No country has yet implemented universal screening for hepatitis B infection. But one analysis8 found that a one-time screening of the entire population could save as many as 23,000 lives and up to US$596 million in health-care expenses in the United States alone, compared with risk-based screening. This could become a reality with policy changes and coordinated efforts by primary-care physicians.
The world’s liver cancer death rate does not need to keep going up — the trend can be reversed with currently available tools. The basic actions that would make a massive difference are getting a handle on who has hepatitis B infection, and making sure that infected individuals receive the monitoring and interventions they require before it’s too late.
Wang says, “I think about the millions of people who could lose out on enjoying life because they simply don’t know they have the virus, and about how lucky I am that my early treatment gave my liver the chance to regenerate itself.” Wang is now a healthy 56-year-old: a living example that liver cancer can be prevented with the right knowledge and care.








More News
Editorial Expression of Concern: Leptin stimulates fatty-acid oxidation by activating AMP-activated protein kinase – Nature
Quantum control of a cat qubit with bit-flip times exceeding ten seconds – Nature
Venus water loss is dominated by HCO+ dissociative recombination – Nature