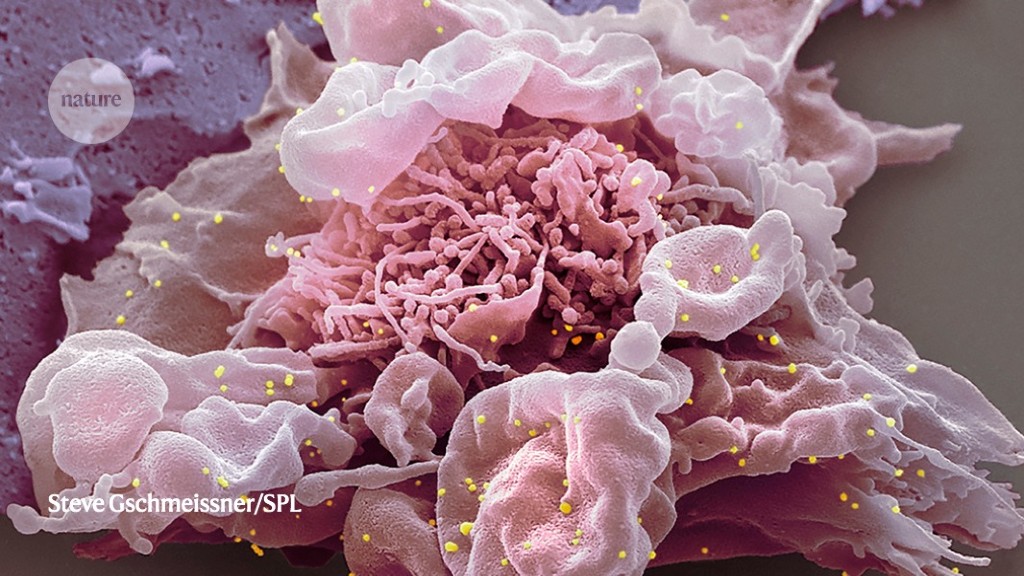
People who become infected with SARS-CoV-2 after three doses of COVID-19 vaccine are much more likely to have the Omicron variant than the Delta variant, owing to Omicron’s ability to evade the immune system, according to US data.
One way in which viral variants can become dominant is by increasing their transmissibility, through faster replication or an enhanced ability to spread outside the body. Another route to dominance uses an increased ability to escape from immune systems that have learnt — through infection or vaccination — to recognize the virus.
Delta achieved its dominance with the former method: the virus could replicate much faster and to higher levels than could previous variants. “Delta did a lot of things through brute force,” says Nathan Grubaugh, an epidemiologist at Yale School of Public Health in New Haven, Connecticut. Omicron seems to replicate even more quickly than Delta, but the number of virus particles in the body never reaches the same level, suggesting that the variant’s advantage lies elsewhere.
Delta vs Omicron
Grubaugh and his colleagues studied the results of 37,877 polymerase chain reaction tests on samples collected in Connecticut over two weeks in mid-December 2021, when Delta and Omicron each made up about 50% of COVID-19 cases in the area. The team determined which variant each test had detected, and correlated those data with the infected person’s vaccination status.
In a preprint1 posted on 25 January, the researchers reported that infected people who either were unvaccinated or had received only one dose of a vaccine were more likely to have Delta than Omicron. But infected people who had received two vaccine doses had almost two times higher odds of having Omicron than Delta, and those who had received three doses had three times higher odds of having Omicron.
That suggests that the Omicron variant is much better than Delta at breaking through the immunity conferred by vaccines. However, the team says that a third, booster shot still cuts the risk of Omicron infection by 50%. The findings have not yet been peer reviewed.
Unpublished work from Grubaugh’s lab suggests that the virus circulating in the bodies of vaccinated people has less genetic diversity than that in unvaccinated people, which implies that vaccines are not promoting new mutations. But as more people acquire immunity through infection or vaccination, viral strains that can evade the immune response will have an increasing advantage over others.
Nathaniel Landau, a microbiologist at New York University Grossman School of Medicine in New York City, says the work supports the idea that an Omicron-specific vaccine would be useful, although he adds that there is always the possibility of a very different strain becoming dominant in the future. A key remaining question, Landau says, is whether something about the biology of the virus makes it more transmissible, as well as better able to evade the immune system. For example, the virus’s propensity to live in the upper airways instead of in the lungs could cause it to spread more easily than Delta.
Vaughn Cooper, an evolutionary biologist at the University of Pittsburgh in Pennsylvania, adds that the function of mutations in Omicron’s spike protein has been a particularly vexing question. “We don’t understand how this weird combination of mutations found in the Omicron spike interacts to escape immunity,” he says. “The sheer number of new mutations makes it hard to pinpoint which combination is the cause.”





More News
AI & robotics briefing: AI decodes languages in first ‘bilingual’ brain-reading device
Mexico’s next president is likely to be this scientist — but researchers are split in their support
Pro-CRISPR PcrIIC1-associated Cas9 system for enhanced bacterial immunity – Nature