In 43 schools across the United Kingdom, groups of teenagers and pre-teens practised paying attention, being in the moment and savouring what is good in life. During weekly sessions that lasted 30 to 50 minutes, more than 3,600 children worked through these teacher-led exercises in a mindfulness-based intervention, called the .b programme. It was supposed to help the children deal with stress, nerves and their worries in ten weekly sessions. But a year after the intervention, the 11- to 14-year-olds in the experiment were no better off on a scale of depression and well-being than those who were taught the usual social-emotional curriculum1. In fact, says psychiatrist Willem Kuyken at the University of Oxford, UK, there was some evidence that children with existing mental-health problems might even have got a little worse.
Adolescent mental health has become a topic of growing concern, and the US Preventive Services Task Force recommends screening all children aged 8 to 18 for anxiety. As mental-health concerns grow, scientists are looking to prevention as a strategy for addressing rising rates of depression among young people. Researchers say it is both possible and essential to ward off mental-health issues, which frequently begin in adolescence. But as programmes that aim to build resilience proliferate in schools, research such as Kuyken’s points to the complexity of the task.
Decades of research paint a complicated picture of an exploding landscape of intervention programmes, studies that are impossible to compare with each other and conflicting results — some discouraging and others more promising. Taken as a whole, the research suggests that there might not be one strategy that will work for all children, but also emphasizes the need to better understand how to address a snowballing crisis in young people, especially girls.
Interventions will probably have to shift focus from schools to the structural societal issues that are straining mental health at a time when kids learn how to form relationships and function in the world, Kuyken says. “We might need a radical rethink of how we think about the promotion of mental health in young people,” he says. “It’s not just about preventing mental-health problems in children. It’s about setting people up for life.”
A depressing trend
Until the mid-1990s, the general consensus in psychiatry was that depression was a condition found only in adults, says Tamsin Ford, a child and adolescent psychiatrist at the University of Cambridge, UK. But it has since become clear that adolescence is a crucial period for mental health. Although children as young as three can be diagnosed with depression, typical onset is in the early teen years, which is a period of intense brain development, Kuyken says. Half of all mental-health disorders begin by age 14, and 75% start by the mid-20s, research shows2. If a young person experiences depression or anxiety, Kuyken adds, that’s often a sign that they might face lifelong challenges with symptoms.
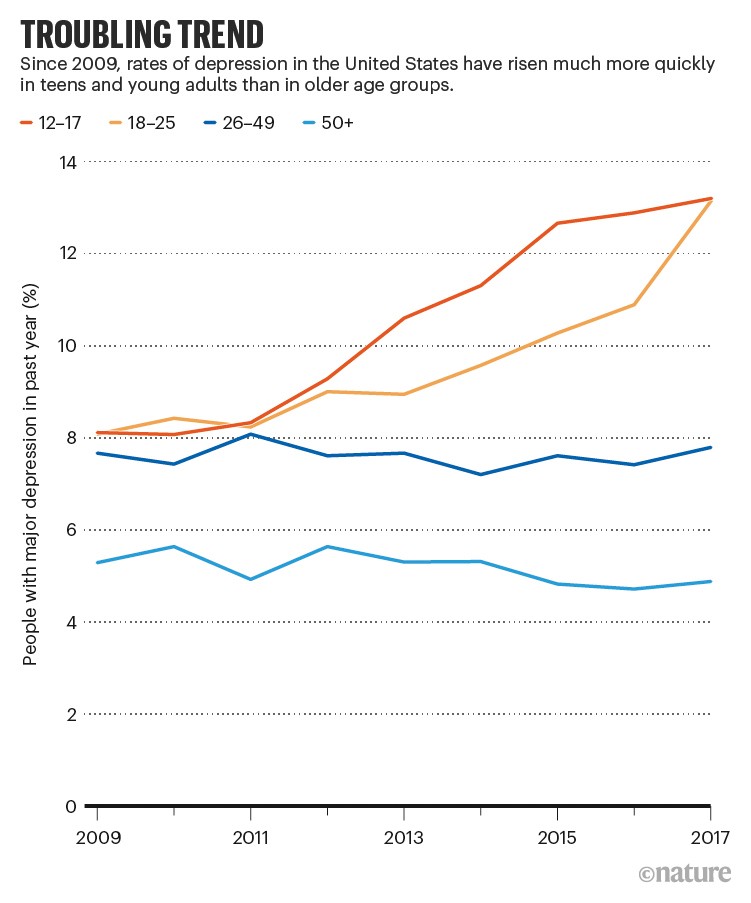
As awareness has grown, so too has prevalence (see ‘Troubling trend’). From 1995 to 2014, rates of self-reported mental-health conditions increased from 0.8% to 4.8% among a sample of more than 140,000 people aged 4 to 24 in England3. Between 2009 and 2019, the number of 12- to 17-year-olds who had experienced a major depressive episode in the past year in the United States increased from 8.1% to 15.8%, according to a recent analysis of data collected from more than 167,000 adolescents by the National Survey on Drug Use and Health4.
Girls are of particular concern. In the US study, rates of depression in teen girls rose from 11.4% to 23.4% — more than triple the 3.7% rise seen in boys. In a representative survey of 26,885 students aged 11–14 across the United Kingdom, as many as 1 in 3 reported significant depressive symptoms5. The reasons for this disparity still aren’t completely clear, says Sylia Wilson, a clinical psychologist at the University of Minnesota Twin Cities, who co-authored a commentary6 about the US study.
The COVID-19 pandemic has put more strain on the mental health of young people. In the United States alone, more than 140,000 children under the age of 18 lost a parent or carer to COVID-19 between April 2020 and June 2021, according to a 2021 study7. Lockdowns caused isolation and family conflict. Among 5- to 16-year-olds, according to a report by the UK’s National Health Service8, rates of probable mental-health conditions reached 16% in July 2020, up from less than 11% in 2017. And across 12 longitudinal studies from the United States, the Netherlands and Peru9, researchers found a moderate increase in depressive symptoms in adolescents in 2020, with the worst outcomes among those living under the most stringent lockdown restrictions.
In some places, researchers are only just starting to document rates of depression and related disorders in young people, as well as how pandemics, wars and other traumatic world events can affect mental health in this age group. Fadi Maalouf, a child and adolescent psychiatrist at the American University of Beirut, and his team translated and validated standard screening questionnaires for depression into Arabic. Maalouf and his colleagues then used the tool to survey a nationally representative sample of more than 1,500 children, aged 5 to 1810. About one-third of the group had at least one psychiatric disorder — a higher rate than other studies have found in a variety of countries such as Nepal (19%) and Germany (14.5%). Depressive disorder showed up in 6% of the participants, and anxiety occurred in 23%.
The findings were the first record of the prevalence of mental-health conditions in Lebanon’s young people, and they offer insight into how traumatic events affect the world’s youth. Several months after a catastrophic explosion in the port of Beirut killed more than 200 people, injured roughly 1,000 children and displaced 300,000 people in August 2020, Maalouf and his colleagues surveyed the parents of roughly 800 children, aged 8 to 17, who had been affected by the incident. One-third of the children showed signs of depression11, five times the normal background rate, which included people already dealing with the pandemic. Nearly two-thirds had symptoms of anxiety, almost three times the typical proportion; 52% screened positive for post-traumatic stress disorder, more than double the rate for children not affected by the blast.
Once a child is diagnosed with depression, treatment options are well established, says Tamar Mendelson, director of the Center for Adolescent Health at the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland. The first-line psychosocial therapies of choice are cognitive behaviour therapy and interpersonal therapy. The class of antidepressant drugs known as selective serotonin reuptake inhibitors (SSRIs), despite concerns about their impact on suicidal thinking, have been shown to help teens; several SSRIs are approved for paediatric patients. Other options, depending on the severity of the symptoms and whether a person’s depression has been resistant to other treatments, include tricyclic antidepressants, electroshock therapy and physical exercise.
Despite the variety of therapeutic paths, 60% of young people with depression in the United States do not receive any mental-health treatment at all, Mendelson says. Even in states with the best access to mental-health care, one in three young people go without treatment. In Texas, the worst state for treatment access, nearly three-quarters of young people with depression are not getting help. Lack of access to treatment is a worldwide problem, and the gaps are extreme in some places, says Maalouf. In Lebanon, according to one study10, just 5% of children with depression sought professional treatment.
Preventive potential
Given how many young people struggle with mental health and how few have access to treatments that can be expensive and time-consuming, schools have become an appealing target for intervention, Kuyken says. Helping kids in a place where they spend so much of their time could theoretically make a big dent in the problem.
Although there are reasons to think that prevention programmes could work in schools, studies have shown that adolescents benefit the most from those that take place in clinics or other health-care settings. In one multi-site study with 316 teenagers, clinical psychologist Judy Garber at Vanderbilt University in Nashville, Tennessee, and her colleagues found lower rates of depression in teens who went through 90-minute group sessions for 8 weeks12. Those benefits persisted when the researchers followed up after six years.
But when it comes to school-based programmes, results are mixed, especially for universal approaches that attempt to teach emotional-coping skills to all children. The most recent Cochrane review of psychotherapy-based prevention programmes, published in 2016, included 83 trials that were conducted mostly in school settings13. The review found no evidence that universal approaches reduced the chances that young people would be diagnosed with depression. There were slightly better results with targeted approaches, which are directed only at children who have a parent with depression or who are at risk for other reasons, or at those who show signs of behavioural or mental-health problems. But trials often had no control groups. The researchers concluded that the evidence wasn’t strong enough to warrant recommending the programmes.
Since then, studies have started to zero in on how specific interventions might be useful for certain populations with a variety of mental-health conditions. Mendelson has studied an intervention called RAP Club, which combines mindfulness and cognitive behavioural strategies in schools serving disadvantaged communities in Baltimore, Maryland. In one study14, groups of 12- to 15-year-olds at two schools participated in 12 sessions that included activities such as shaking up a bottle of fizzy drink and then opening it to illustrate how it feels to explode with emotions (an activity preceded by the donning of waterproof ponchos). In unpublished data, Mendelson and her colleagues found that, four months later, the students who had been through the programme had fewer trauma symptoms and reported more success at dealing with stress. RAP Club didn’t immediately make a difference in depression or anxiety symptoms, Mendelson concedes. But when the COVID-19 pandemic started several years after the study had ended, the researchers checked back in and, according to still-unpublished data, they found lower rates of anxiety — and a trend towards less depression — in students who had completed the programme than in those who had not.
Other promising results have emerged from studies in a variety of countries. Researchers in Norway, for example, delivered a strategy that teaches emotion regulation and other skills to more than 800 students, aged 8 to 12, who were flagged by a screening test with elevated symptoms of depression and anxiety15. Students who received the intervention — called EMOTION — had almost twice the reduction in symptoms compared with a control group of students who did not participate in the programme. In Lebanon, Maalouf and his colleagues tested the FRIENDS programme, a resiliency curriculum developed in Australia that uses cognitive behaviour therapy techniques to prevent anxiety and depression. They translated the programme into Arabic, then delivered it to 280 students aged 11 to 13, at 10 schools in Beirut as part of a randomized trial16. After 10 sessions in the classroom over 3 months, children who received the intervention showed improvement in depressive and emotional symptoms compared with the control group. Girls also showed a reduction in anxiety.
Despite those successes, studies continue to flag the need for better data. A 2021 meta-analysis17 concluded that preventive interventions can be successfully delivered in schools, workplaces and community settings — but that more well-designed studies are needed before the evidence will be convincing enough to recommend universal prevention programmes for all.
The nuances are plentiful. Although Kuyken’s large UK mindfulness study1 found no benefit for children, teachers reported lower levels of burnout after going through the training18. Students with teachers who were best at leading the programme were more likely to do the exercises19. And teachers who participated reported improvements in the school climate, which included an atmosphere of respect18.
There are multiple reasons why studying prevention in schools is complicated. Schools are variable environments. Studies are often small, lacking control groups, and include only short-term follow-up. Depression itself is a heterogeneous condition, Garber adds. And kids can vary in their willingness to participate in group activities.
It can also be hard to gauge what prevention means, especially when a programme might have short-term gains that don’t last forever. Garber compares prevention programmes with vaccines that require booster shots as children face new stressors throughout life. “If you’re going to prevent depression, you have to engage in these kinds of skill that we’re trying to teach people, but it’s not a one-time thing,” she says.
With multiple studies in progress, more answers should be on their way, says Joan Luby, a child psychiatrist at Washington University School of Medicine in St. Louis, Missouri. And researchers might eventually find that interventions need to start earlier. In her work with young children, Luby and her colleagues have modified interactive parent–child therapy, normally used as a treatment, into a preventive intervention for preschool children, which they adapted to deliver by Zoom throughout the pandemic. They plan to test the programme as a depression-prevention strategy in primary-care offices and in schools across the St. Louis area.
The goal is to address “emotional development early in life in a healthy fashion, teach children to learn to experience pleasure from events, learn to sustain those positive emotions, learn to regulate negative emotions, learn not to selectively attend to negative emotions”. Achievement of those aims “might set the developmental trajectory on a healthier path”, Luby says, adding: “we still have to prove that”.
To be more universally effective, efforts to prevent depression might ultimately need to demand less of teachers and kids, and focus more on poverty, violence, homelessness, food insecurity and other structural problems that affect children’s mental health. “We are too quick to see the problems with children and the solution with children,” Kuyken says. “If a kid is arriving at school not having had breakfast or not having access to Wi-Fi so they can’t do their homework, learning psychological techniques for mental health is not really cutting the mustard. Maybe what we need to be doing is not looking at the kids’ resilience, but the causes of the kids’ distress in the first place.”






More News
Could bird flu in cows lead to a human outbreak? Slow response worries scientists
US halts funding to controversial virus-hunting group: what researchers think
How high-fat diets feed breast cancer