Now what?
After the Omicron variant brought a fresh wave of SARS-CoV-2 infections and anxiety at the start of 2022, some nations are starting to record a decline in case numbers. But after two years of oscillating between pandemic surges and retreats, even people in these countries cannot help but wonder when the next blow will come — and what form it will take.
“I think it is inevitable that we will see new variants with varying degrees of immune evasion,” says Andrew Rambaut, who studies viral evolution at the University of Edinburgh, UK. “They could emerge from wherever there is widespread transmission.”
As they wait for the next variant to enter the scene, scientists are studying the currently dominant Omicron variant to better predict the future; this research is described in a separate Feature. Here are three key questions scientists would like that research to answer.
When will the next variant of concern emerge?
There is no way to know for sure when a variant will become dominant, or whether it will rise to the status of a ‘variant of concern’ — meaning that there are signs that it has picked up worrying new properties, such as spreading more rapidly, causing more-severe disease or evading immune responses.
The public is most familiar with the first dominant sub-variants of Omicron and Delta. But researchers have been tracking a host of related sub-variants that are jockeying for dominance. In the United Kingdom, for example, one Delta variant called AY.4 was in the process of being rapidly displaced by another, called AY.4.2, in late 2021. “And then Omicron came along and just blew up,” says bioinformatician Andrew Page at the Quadram Institute in Norwich, UK.
The history of these viral dynamics suggests that a new variant will sweep through every few months, says Page. “They seem to happen quite regularly,” he says. “It’s probably just going to tick along.”
But whether that variant will rise to the level of a variant of concern remains an open question. At present, the original BA.1 Omicron lineage is being replaced by another, called BA.2. This lineage, although probably more transmissible than BA.1, does not seem to be a major change from the original one that swept through many countries earlier this year.
Such dynamics are probably common in viral pathogens. But the world has not followed a viral infection so closely before, says Page, and as a result, scientists had been missing out on the fine print. That close scrutiny, however, is already diminishing: COVID-19 testing rates in the United Kingdom have declined, he notes, in part because Omicron tends to produce relatively mild disease. With a mild disease, people are less likely to seek testing, and governments become less proactive in encouraging tests.
Eventually, this will weaken SARS-CoV-2 genomic surveillance efforts. When Omicron was discovered, the alarm was sounded very quickly, Page says, but in the future, it could take weeks longer to realize a new variant of concern is afoot. “There’s no way that we can keep up the pace we’ve had so far,” he says. “But if it’s not causing severe disease, do you need to have such intense surveillance?”
Will the next variant cause severe disease?
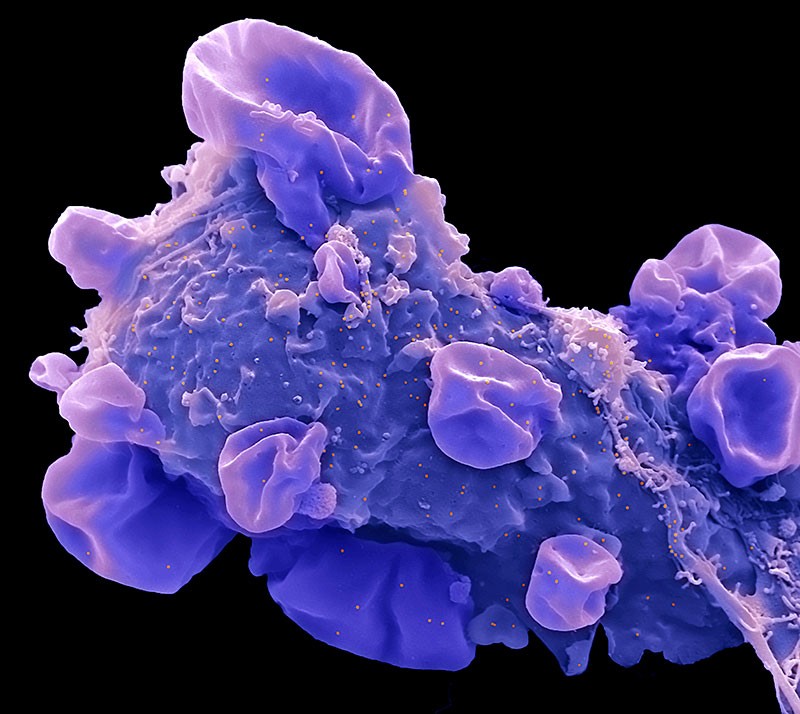
Omicron is less likely to cause severe disease than previous variants of concern — a feature that has helped to temper the impact of the variant’s rampant spread.
Although that has fed speculation that the virus could be evolving towards a strain that induces a milder disease, SARS-CoV-2’s evolutionary path remains unclear, says Rambaut. Thus far, new variants of concern have not evolved from the dominant preceding one. Instead, they have emerged from separate lineages. There is no guarantee that the next dominant variant will sprout from the ‘mild’ Omicron branch of the SARS-CoV-2 family tree. “It is possible that a later variant may be back to a Delta or Alpha lineage, with sufficient immune evasion to sweep Omicron away,” says Rambaut.
Researchers also still don’t know the extent to which Omicron’s relative mildness is due to the prevalence of immunity against SARS-CoV-2, rather than intrinsic properties of the virus itself. As more of the world’s population becomes vaccinated, infected or both, immunity is likely to grow and so, too, will resilience against severe COVID-19.
But there were some differences in how Omicron behaved compared with previous variants, notes immunologist Wendy Burgers at the University of Cape Town in South Africa. Several animal studies, for example, have found that Omicron is less likely to affect the lungs, than previous variants1. “Will the next mutated variant have different properties?” she says. “I don’t think there’s any guarantee that those intrinsic differences might not be worse.”
“We know a lot about the humans, but it’s the virus that’s unpredictable,” she says. “And I’m a little scared of that.”
Will vaccines protect against emerging variants?
The 54 mutations in Omicron’s genome — and particularly the 34 clustered in a key viral protein called spike — severely weakens the ability of COVID-19 vaccines to prevent SARS-CoV-2 infection. But protection against severe disease seems to have remained high, and probably contributed to the perceived mild disease caused by Omicron.
That bodes well for the resilience of vaccine-mediated immunity against future variants of concern, says Burgers. Although Omicron’s spike mutations seem to weaken antibody defences, scientists have detected only slight declines in the ability of immune cells called T cells to recognize the virus. These cells are thought to be particularly important in limiting the scope of a viral infection, killing off infected cells and limiting the virus’s spread. “I really breathed a sigh of relief after Omicron,” Burgers says. “I’m optimistic that the T-cell response will be quite resilient even if a new variant emerges.”
But Burgers notes that as antibodies become less relevant for SARS-CoV-2 immunity, T cells become more important, and a viral variant that can evade T-cell surveillance will have a key survival advantage. “The T-cell response is doing much more of the heavy lifting,” she says. “So one thing we might start seeing is T-cell escape.”
In other viruses, such as influenza, the ability to escape T-cell immunity develops gradually over the course of years. But it’s hard to predict how quickly it will proceed in the middle of a raging pandemic, Burgers says.
It is also becoming more difficult for immunologists to anticipate how population immunity will shape the course of the pandemic, as the drivers of that immunity grow increasingly complex. People might have received one of a number of vaccines, or a combination of vaccines, or experienced an infection from one or more variants, with or without vaccination.
In general, this accumulation of exposures to SARS-CoV-2 variants should boost immunity, says infectious-disease specialist Santiago Ávila Ríos at Mexico’s National Institute of Respiratory Diseases in Mexico City. In a preprint, Ríos and his team reported that multiple exposures to SARS-CoV-2, either through vaccination or infection, amplified antibody responses, as well as responses by immune cells called B cells2. “Thus, as more persons become exposed to the virus through different mechanisms, the emergence of new variants of concern may impose a lower disease burden,” he says.
But some types of exposure might be better than others for preparing the body to fight off new variants. One study3, which has not yet been peer reviewed, found that people who had been vaccinated and then were infected with Omicron experienced “whopping increases in antibodies”, says virologist Penny Moore at the University of the Witwatersrand in Johannesburg, South Africa. Those antibodies could attach to and disarm multiple SARS-CoV-2 variants besides Omicron, a property called cross-reactivity.
But antibodies produced by people who have been infected with Omicron but not previously exposed to SARS-CoV-2 — either by vaccination or infection — were not as robust in blocking other variants. “We can’t assume that those people would be particularly well protected against incoming variants of concern,” Moore says.
Ultimately, the data continue to point to the importance of vaccination, says Burgers. “We know that vaccines shore up our immunity and that immunity will be cross-reactive, when it comes to T cells, with another variant,” she says. “There’s a lot that we don’t know, but there’s a lot that’s in our control.”

More News
Daily briefing: Carrion crows have counting skills seen only in people
Researcher parents are paying a high price for conference travel — here’s how to fix it
Asymmetric hydrogenation of ketimines with minimally different alkyl groups – Nature