When Stavros Lomvardas came down with COVID-19 earlier this year, he monitored his symptoms closely. Lomvardas, a neuroscientist at Columbia University Irving Medical Center in New York City, had just wrapped up a study of how SARS-CoV-2 infections cause loss of smell1. “Quite frankly,” he says, “I was very curious to experience it.”
But Lomvardas didn’t get severely ill — and, unlike many who had COVID-19 at the start of the pandemic, his olfactory functions remained intact. He had no trouble enjoying food, gauging personal hygiene or engaging in other everyday activities that require smell.
Lomvardas probably contracted the Omicron variant: a form of SARS-CoV-2 that is often milder than variants such as Delta, and which affects smell in less than one-quarter of those infected. Yet, even as loss of smell — known as anosmia — becomes less common than it was earlier in the pandemic, “this doesn’t mean the problem is disappearing”, says Rafał Butowt, a neuroscientist at Nicolaus Copernicus University in Bydgoszcz, Poland.
The virus could evolve again to spur on anosmia with a vengeance. And one soon-to-be-published study estimates that among those who already have COVID-induced smell loss, 1 in 20 people will never get it back. Treatments to restore the sense are desperately needed, says Zara Patel, a sinus surgeon at Stanford University School of Medicine in California. “There’s really a dearth of knowledge or management options,” she says.
The impact of such treatments could even extend beyond the nose and into the brain: post-mortems and brain scans have linked COVID-19-related tissue damage to the olfactory system. But as Butowt points out, there are still a lot of open questions about the biological mechanisms behind COVID-related anosmia.
Teasing apart those mechanisms is now a priority for olfactory researchers. Work to gain a better understanding of what the virus does in the nasal cavity, and why variants seem more or less likely to cause anosmia in different people, is advancing. Scientists are also getting closer to uncovering treatments to address post-COVID smell dysfunction in the process.
Nervous breakdown
The question of whether SARS-CoV-2 can infect sensory neurons in the nose has divided researchers since the beginning of the pandemic. Several other viruses, including those responsible for influenza, herpes and polio, are known to gain entry to those neurons, prompting not only anosmia but also neurological complications. That’s because olfactory neurons are connected through nerve fibres to smell-processing centres in the brain — and viruses can use the olfactory nerve as a shortcut into the central nervous system, often with devastating consequences.
It seemed logical that, given early reports of smell loss linked to SARS-CoV-2, the coronavirus would gain access to the olfactory pathway in the same way. But when two teams — one led by Butowt2, and the other by neurobiologist Sandeep Robert Datta at Harvard Medical School in Boston, Massachusetts3 — looked for signs of a protein known as ACE2, used by the virus to gain passage into cells, they found scant evidence of it in the neurons.
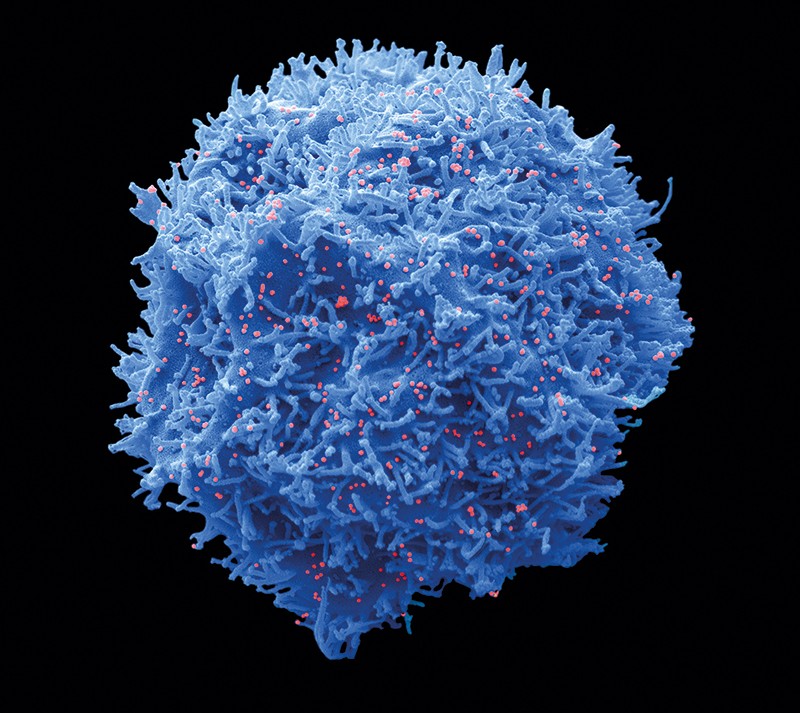
Rather than neurons themselves hosting the virus, it seemed that the viral conquest of surrounding support cells was to blame. In particular, rhinologist Andrew Lane and his colleagues at the Johns Hopkins University School of Medicine in Baltimore, Maryland, showed that sustentacular cells, which surround the smell-sensing neurons in the olfactory epithelium, are full of ACE24.
These support cells normally aid neurons in recognizing odours. But once infected, they start to shed the virus and destruct, setting off alarm bells for the immune system. Inflammation kicks in, and the resulting hot mess of immune signalling ultimately destroys nearby neurons’ ability to detect and transmit odour information to the brain.
Clinical support for the idea that sustentacular cells, not neurons, are the prime target of SARS-CoV-2 attack in the upper nose comes from an analysis of post-mortem tissue samples from 70 people who had died with or from complications of COVID-195. The research team was led by rhinologist Laura Van Gerven at the Catholic University of Leuven in Belgium and olfactory scientist Peter Mombaerts at the Max Planck Research Unit for Neurogenetics in Frankfurt, Germany. They meticulously searched for signs of SARS-CoV-2 in cells that line the roof of the nasal cavity, and regularly saw hallmarks of infection in sustentacular cells — including evidence of continuing viral replication in some cases. “But no matter how hard we looked,” says Van Gerven, “we could not find any evidence that there was indeed infection of the olfactory neurons.”
Lomvardas took this finding one step further. Working with virologist Benjamin tenOever at New York University Langone Health in New York City, he too showed that the neurons were almost virus-free, both in hamsters and in human tissues1. But the team also showed that those neurons were receiving signals from nearby infected cells, which prompted the neuronal genomes to undergo a drastic organizational overhaul.
With gene expression in disarray, the receptor proteins — which are needed to detect different odorants — were never made, tenOever says, resulting in “a total loss of bandwidth in the neurons”. A hamster study led by neurobiologist Nicolas Meunier at the National Research Institute for Agriculture, Food and Environment (INRAE) in Jouy-en-Josas, France, implicated a group of immunological first responders, known as neutrophils, in mediating this destructive cascade6. And a study involving single-cell profiling of nasal biopsies from people living with persistent post-COVID smell loss suggested that a population of T cells also contributes to inflammation7. According to Bradley Goldstein, an otolaryngologist at the Duke University School of Medicine in Durham, North Carolina, who led the study alongside Datta, the presence of these T cells “likely reflects immune dysfunction that is preventing full recovery” in some people with long-term olfactory problems after COVID-19.
But not everyone agrees that inflammation, rather than direct infection of neurons, is to blame for anosmia. Several autopsy reports have identified SARS-CoV-2 inside nerve cells of the nose, and one group studying the olfactory mucosa of people living with persistent COVID-associated anosmia reported that the virus does find its way into smell-sensing neurons8 — albeit possibly after other cells in the nasal environment were infected.
Marc Lecuit, a microbiologist and infectious-disease physician at the Pasteur Institute in Paris, who co-led the study, thinks that inflammatory assault as well as viral infection probably play a part. “There’s good reason to believe it’s the combination of both that contributes to anosmia,” he says.
Sensory difference
Whatever the mechanism, not everyone who tests positive for COVID-19 loses their sense of smell — and researchers are beginning to work out why. A person’s genetic make-up is one contributing factor. A study published earlier this year by researchers at 23andMe, a personal genomics company in Sunnyvale, California, found that people with particular variations in a gene connected to odorant metabolism were especially prone to losing their sense of smell owing to COVID-199.
Underlying health conditions can come into play, too. In unpublished work, neurobiologist Katja Kanninen at the University of Eastern Finland in Kuopio says she and her colleagues found that when nasal tissue from people with Alzheimer’s disease was exposed to SARS-CoV-2 in vitro, gene expression in the cells went haywire — more so than in cells from healthy people. “They mount a kind of augmented response to the virus,” she says. This could explain why some people experience greater olfactory effects and cognitive impairment after COVID-19.
Properties of SARS-CoV-2 itself, such as genetic changes acquired over the course of viral evolution, can also affect the impact on olfactory tissues. At the beginning of the pandemic, a mutation popped up at position 614 of the virus’s spike protein and this variant quickly spread across the globe. Butowt and neuroscientist Christopher von Bartheld at the University of Nevada School of Medicine in Reno have found that this tiny genetic tweak increased people’s risk of developing post-COVID anosmia, perhaps because it made the virus better at infecting support cells in the nasal cavity10. The mutation is now found in every variant of concern, including Omicron.
Many more genetic alterations have followed, and it is still unclear why the constellation of dozens of mutations found in the Omicron variant enable it to spread with increased vigour and yet provoke the loss of smell much less frequently than did earlier forms of the virus. Butowt and his colleagues have proposed that Omicron’s many mutations might alter the physical properties of the spike protein in ways that hamper SARS-CoV-2’s ability to either penetrate mucus barriers in the nose or enter sustentacular cells.
Alternatively, it could be that Omicron is so good at commandeering cells of the respiratory tract that it simply takes root in the first tissues it encounters — in the back of the throat, for instance — and never makes its way to the olfactory cells in the upper nasal cavity. This would also explain why Omicron is less prone to wreaking havoc in the lungs. Lane has observed this type of confined infection in respiratory cells in hamsters11. “This correlates with the clinical observations of high transmissibility and less frequent olfactory loss,” he says.
Deciphering the ins and outs of nasal infection could inform clinical management of anosmia and other post-COVID complications. Current treatment options are limited, with none tailored to the biology of SARS-CoV-2. “There is a need for better targeted therapies,” says Carol Yan, a rhinologist at the University of California, San Diego.
On the basis of his team’s latest data12, tenOever suspects that a type of anti-arthritic drug known as a JAK inhibitor — which targets enzymes in the Janus kinase family to prevent communication through pro-inflammatory signalling molecules — could help to quell immune responses in the nose. “That has great potential,” tenOever says, “but it would not have been my obvious go-to if we had not known the mechanism.”
After tenOever reported his initial findings in February, he says he was “inundated” with e-mails from people who were experiencing long-term post-COVID anosmia. Reading their stories of persistent smell dysfunction has redoubled his interest in unravelling the mechanics of the process. He started studying the links between SARS-CoV-2 and olfaction largely out of academic curiosity. But now, he says, “I’m doing it more for those people, because I feel for them.”





More News
Audio long read: How does ChatGPT ‘think’? Psychology and neuroscience crack open AI large language models
Ozempic keeps wowing: trial data show benefits for kidney disease
What steps to take when funding starts to run out