A trial in Sweden showed that uptake rates rose slightly if people were given 200 krona (US$24) to have a COVID-19 vaccine.Credit: Karol Serewis/SOPA Images/LightRocket/Getty
Around the middle of 2021, some governments around the world began to get creative with their COVID-19 vaccination programmes. Eager to get vaccines into as many arms as possible, they began to offer unusual incentives: in San Luis, Philippines, vaccinated residents could enter a sweepstake to win a cow; in Hong Kong, the windfall was an apartment; in West Virginia, it was a hunting rifle, among other prizes.
Evidence about the effectiveness of such efforts is mixed1, and the research that has been done suggests that guaranteed, immediate payments are more effective than gimmicks and lotteries2. A randomized trial in Sweden in 2021, for example, showed that a cash payment of 200 krona (US$24) to those receiving their first dose of a COVID-19 vaccine was enough to drive up vaccination rates by 4.2 percentage points3.
Read the paper: Financial incentives for vaccination do not have negative unintended consequences
However, people and policymakers still worry that such incentives could have unintended negative consequences. People might expect payment for future vaccinations, for instance. Or they might think the payments are compensation for something that isn’t safe or could be unpleasant. Now, the results of two trials published in a paper on 11 January in Nature suggest that simple cash payments have no such unintended effects4. The research team took the important step of designing the studies to test a null hypothesis. This gave them the statistical power to detect the absence of an effect, and not just document a lack of evidence for negative consequences. Such studies (including testing a null result) add to the discussion around financial incentives for vaccination and highlight the value of strong research for policy-relevant questions.
Financial incentives — and disincentives — have long been used to achieve public-health goals, but as a general rule, they have targeted mostly unhealthy behaviours. Take, for example, taxes on cigarettes to discourage smoking. Randomized trials indicate that direct cash payments can be effective in stopping smoking during pregnancy5.
But there’s been a long-standing worry that offering payments for vaccination could reduce people’s trust in the safety of vaccines, erode their sense of altruism and make it difficult to implement future vaccine programmes without payments. Although these concerns are largely theoretical, they have led some policy advisers to recommend against implementing programmes that offer cash to promote healthy behaviours. The authors of the Nature paper, a team of economists from Europe and the United States, address such concerns head on by analysing data from randomized studies of more than 2,700 people involved in the Swedish cash-incentive programme and of 3,000 people in the United States.
How COVID vaccines shaped 2021 in eight powerful charts
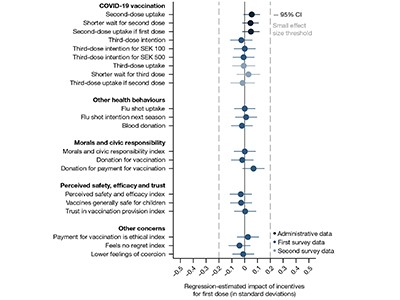
As well as gathering data on second-dose uptake, the Swedish study also surveyed attitudes towards vaccines and other health behaviours. The US study looked at whether informing participants about the existence of incentive programmes that offer public funds for COVID-19 vaccines affected their perception of the products’ safety or efficacy, their sense of civic responsibility or their intention to get an influenza shot or donate blood. Overall, there was no difference in any of these parameters. Nor did participants report feeling coerced by the incentives.
No single experiment can completely answer questions about unintended consequences, and this study, like any other, has its caveats. Ethical requirements dictated that all participants knew they were part of an experiment, and it is possible that this knowledge coloured their responses to survey questions. The results also might not apply to other countries or other vaccines: the COVID-19 pandemic is unique in its pre-eminence as well as its politicization, and both regions studied are high-income, Western countries. Nor does this study address wider and more fundamental ethical questions around paying people to get vaccines.
And although the results support the idea that monetary incentives can be deployed without unintended negative consequences, they do not suggest that such approaches should be prioritized over improving access to vaccines when there are insufficient resources to do both. Efforts to build trust or make it easier for people to receive vaccines — by translating information about inoculations into different languages, for example, or bringing vaccination centres closer to the populations most in need — are well-established ways to boost vaccination rates and, in some cases, could cost less than offering financial rewards.
But for communities that have the resources to both bolster access and provide incentives, the latest work brings important data and a rigorous approach to a discussion that has been heavily influenced by untested assumptions about hypothetical negative consequences. More such studies are needed on effective approaches for policy-relevant questions. In the case of vaccines, such information can be harnessed to help health-care providers design alternative ways to promote vaccination — before another pandemic again entices governments to get ahead of the science and become creative.








More News
Judge dismisses superconductivity physicist’s lawsuit against university
Future of Humanity Institute shuts: what’s next for ‘deep future’ research?
Star Formation Shut Down by Multiphase Gas Outflow in a Galaxy at a Redshift of 2.45 – Nature