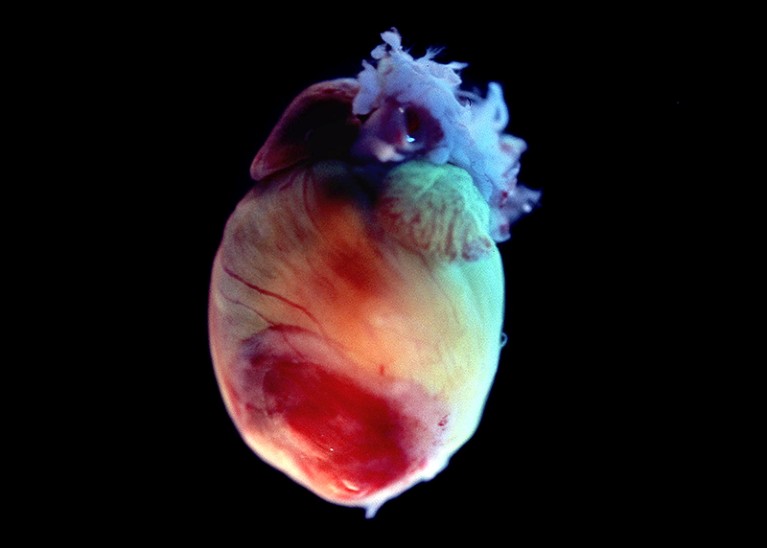
The heart of a mouse. Raising a mouse’s heart beat raises its anxiety level.Credit: Volker Steger/Science Photo Library
Emotions such as fear and anxiety can make the heart beat faster. Now a study in mice has found that the reverse is also true — artificially increasing the heart rate can raise anxiety levels1.
Links between emotions and physical sensations are familiar to everyone: hairs rising on the backs of your arms when you hear an eerie sound, or the sinking feeling in your gut when you receive bad news. But the question of whether emotions drive bodily functions or vice versa has long vexed researchers, because it is hard to control either factor independently.
“It was a chicken-and-egg question that has been the subject of debate for a century,” says Karl Deisseroth, a neuroscientist at Stanford University in California. He learned about this conundrum — first proposed by the psychologist William James in the 1880s — while at medical school and says the question has haunted him ever since.
Well-dressed mice
To test the phenomenon directly, Deisseroth and his colleagues turned to optogenetics, a method that involves using light to control cell activity. The team bioengineered mice to make muscle cells in the rodents’ hearts sensitive to light. The authors also designed tiny vests for the animals that emitted red light, which could pass through the rodents’ bodies all the way to their hearts. When a mouse’s vest emitted a pulse of light, the animal’s engineered heart muscles fired, causing the heart to beat.
The team trained the animals to expect a shock if they pressed a lever for a water reward. Using the optogenetic system, the team raised the animals’ heart rates from their normal 660 beats per minute to 900. When their hearts started racing, mice became less willing to press the lever or to explore open areas, suggesting that they were more anxious. But for animals in other contexts, the externally increased heart rate had no effect, suggesting that the brain and the heart worked together to produce anxiety.
What the heart knows
When the researchers measured the animals’ brain activity, they found that the insula — a region associated with both emotion and the processing of bodily signals — became more active when the heart rate increased if the animal was acting anxious. The researchers say this suggests that the insula is in charge of integrating signals from the heart with threats from the environment before passing the information on to areas involved in higher cognition.
The work “is a major advance in terms of methodology”, says Hugo Critchley, a psychiatrist at Brighton and Sussex Medical School in Sussex, UK. It’s possible, he says, that this heart–brain loop evolved to help animals process danger signals more quickly: when the animal sees a potential threat, even before the brain can fully process what the situation means, the heart rate rises, essentially telling the brain that it should be worried.
The finding could have implications for the treatment of chronic anxiety conditions, says Sahib Khalsa, a psychiatrist at the Laureate Institute for Brain Research in Tulsa, Oklahoma, who studies the link between organ systems and anxiety in humans. Purposely slowing one’s breathing, for instance, has long been known to help reduce anxiety. “There’s a lot of use of these strategies and a sense that [they have] a benefit, but what exactly is doing the anxiety reduction is not well established,” he says. It’s also not clear, he adds, whether acute fear — such as fear of a foot shock — involves the same body–brain circuits as chronic anxiety, which in humans seems to involve more parts of the brain than acute fear does.
Body of emotions
“I just love this paper so much,” says Sarah Garfinkel, a neuroscientist at University College London. Mental-health research that focuses on brain circuitry hasn’t fully answered questions about how mental disorders arise, she says, but studying other organ systems might provide a more complete picture. “You can’t just look at the brain if you want to understand fear,” she says.
Hope that psychedelic drugs can erase trauma
Garfinkel’s own research2 has shown that people can learn that a light flash predicts a painful shock in a ‘dangerous room’ but not in a ‘safe’ room. But people with post-traumatic stress disorder have difficulty calibrating their fear to the threat posed by the room
Deisseroth says he wants to use optogenetics to look at how the brain and behaviour are affected by stimulation of other organ systems, including the gut, the skin cells that raise an animal’s hairs when it confronts a threat, and even facial muscles that are involved in forming expressions and might also play a part in directing emotions.






More News
Diana Wall obituary: ecologist who foresaw the importance of soil biodiversity
These parrots go on killing sprees over real-estate shortages
How the cauliflower got its curlicues