GrayMatters Health is a spin-off from Tel Aviv University in Israel, and one of the final eight for The Spinoff Prize 2021.
Tension builds in the crowded emergency department. Voices grow louder. A baby cries. People rise from their seats and march up to the receptionist’s desk. The scene grows more intense, and the person controlling it — a soldier about to leave for a war zone — isn’t even in the room.
She watches the chaos play out from her seat in a laboratory. The scene is a virtual environment that, thanks to an array of electrodes placed on the soldier’s scalp, reflects her own emotional state. As she practises regulating her reactions, and therefore controlling her neural activity, the virtual waiting room quietens down. People sit. The noise becomes hushed. Calm prevails.
In one study, military trainees underwent experiences similar to this to test whether the virtual environment could help them to regulate their actions on the battlefield1. Psychiatrist Talma Hendler at Tel Aviv University, Israel, and her colleagues found that the trainees became more emotionally resilient than control groups — something that could make them less likely to develop post-traumatic stress disorder (PTSD) after combat.
This form of training the brain, known as neurofeedback, has long been used to treat conditions such as PTSD. The brain, however, doesn’t provide us with sound or visual cues for emotions. So controlling mental processes to curb the brain’s response to an event is a matter of chance, akin to fumbling in the dark to turn off an alarm with no cues to guide you to the right buttons. People can struggle to control their emotional reactions, says Oded Kraft, who co-founded GrayMatters Health in Haifa, Israel, to move the technology out of the laboratory and into clinical care. “This system sort of places a mirror in front of the brain,” he says.
The company’s eventual goal is to prevent people from ever developing PTSD, but first it intends to use the technology to help treat people with PTSD or chronic depression. Globally, more than 250 million people have one of these conditions. This number is likely to grow in the wake of the COVID-19 pandemic, because more paramedics, physicians and nurses are now at risk of mental-health conditions, including PTSD.
Despite the increased need, treatments — drugs and psychotherapy — have remained constant for nearly 40 years, says psychiatry researcher I-Wei Shu at the University of California, San Diego. He adds that for 30–60% of people with a mental-health condition, both are less than ideal: drugs cause unwanted side effects, and psychotherapy frequently requires people to relive traumatic experiences, such as sexual violence, making it a tough metaphorical pill to swallow. “These treatments save the lives of some patients, but most don’t get as much out of them as we’d like,” Shu says. “It’s very important that we mobilize resources to create the next generation of treatments.”
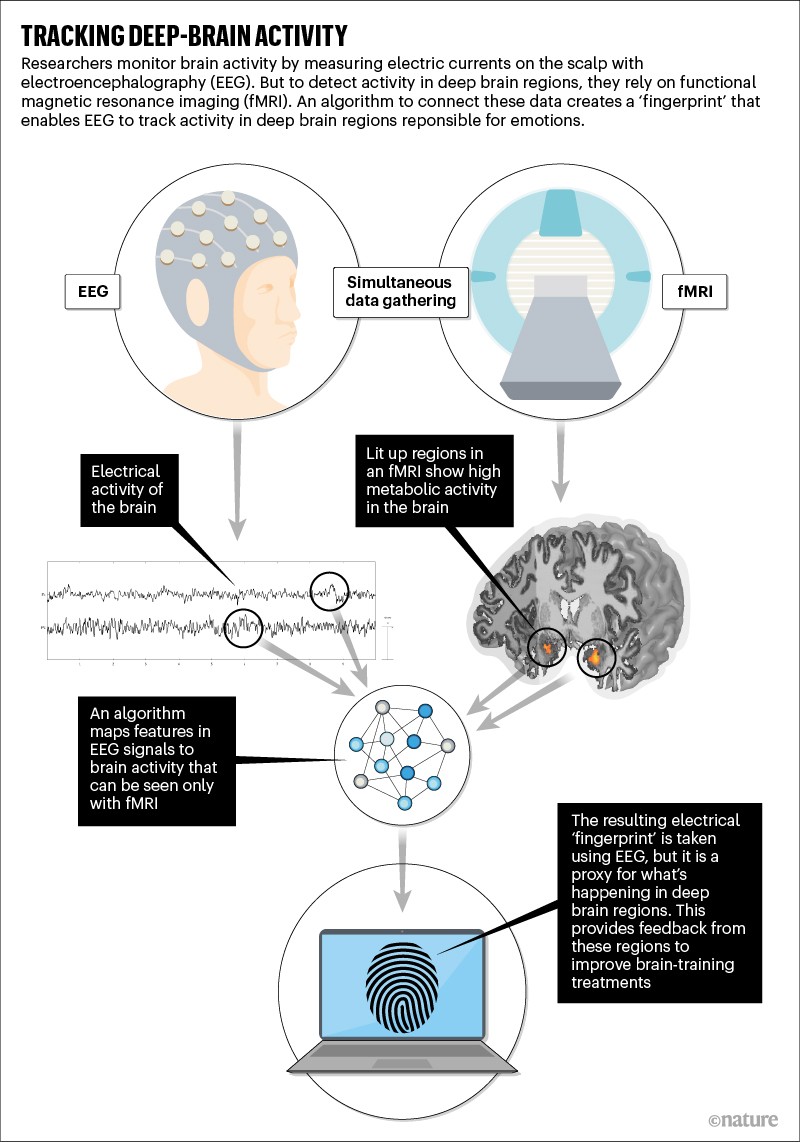
Hendler, who is also the chief medical scientist at GrayMatters Health, began developing one such advance nearly a decade ago, by combining two techniques: electroencephalography (EEG), which has long been used to measure the brain’s activity by tracking electrical currents on the scalp, and functional magnetic resonance imaging (fMRI), which detects brain activity by tracking blood flow. Researchers’ ability to image the brain with fMRI has revolutionized neuroscience by illuminating deep-seated brain regions such as the amygdala — an area crucial to emotions such as fear and anxiety — with unprecedented detail. But the technique requires expensive MRI machinery, typically located in hospitals or medical centres.
An important connection
In 2016, Hendler and her team devised a machine-learning algorithm that allowed them to connect EEG signals to fMRI data. The researchers began by measuring both fMRI and EEG information simultaneously in a group of healthy participants. Putting the data together allowed the researchers to connect the dots between changes in blood flow in the amygdala, measured by the fMRI, and electrical signals on the scalp. The algorithm analysed both kinds of data to create an electrical ‘fingerprint’ that correlated with spikes and troughs in the activity of the amygdala. This fingerprint is measured solely using EEG, but serves as a stand-in for fMRI signals of amygdala activity (see ‘Tracking deep-brain activity’).
The team then set out to validate this fingerprint — would an EEG informed by fMRI data prove better than a standard EEG that tracked only superficial brain regions? With the fingerprint handy, the researchers no longer had to use fMRI on every participant.
The researchers asked participants to use mental strategies to lower the volume of a sound clip they heard. An array of electrodes simultaneously tracked the electrical fingerprint of their amygdala activity. The instructions on how to lower the volume were intentionally vague so that each person came up with a strategy that worked for them, such as deep breathing or visualization. A control group did the same exercise but received feedback only about surface EEG signals — not about how their amygdala was responding. Participants who received feedback about their amygdala activity were significantly more efficient at lowering the volume than were those in the control group2.
The company’s product doesn’t require an fMRI reading — measuring an individual’s EEG fingerprint reflects the deeper workings of their brain, and this fingerprint is accessible through a single surface electrode placed on the scalp. Although EEG-based neurofeedback therapy is widely available, it relies mainly on neuroscience research dating back to the 1970s, not on newer, fMRI-based views of neural activity. Hendler and her team “found a way to connect EEG signals with current models of brain function”, Shu says. “It was unclear how to do this analytically — that’s where they succeeded and others have stalled.”
In addition to the study testing their approach as a preventive strategy for PTSD, Hendler and her colleagues also tested its effectiveness for managing chronic pain owing to fibromyalgia3. In that work, 34 participants received biweekly neurofeedback training for five weeks. People whose sessions were based on the amygdala fingerprint reported better sleep and reduced pain compared with those in the control group. “That was our first demonstration of clinical applications,” Hendler says.
The company secured its first round of funding in February 2020. Around nine months later, its first machines were being tested at Israeli and US universities. The company’s product is classed as an investigational medical device in the United State, which means it is yet to be approved by the US Food and Drug Administration and is accessible only as an adjunct to standard treatments for PTSD and depression. Eventually, Kraft and Hendler foresee wider applications — by studying different brain regions, they could identify electronic fingerprints that correlate with other mental-health conditions.
The company’s technology has the potential to be affordable and accessible at small clinics, not just large hospitals, says Kymberly Young, a neuroscientist at the University of Pittsburgh in Pennsylvania, who is not involved with the start-up. But the company’s future trials will need to compare this form of neurofeedback with other treatments for training the brain to regulate emotions, including drugs and psychotherapy.
Young points out that although the company’s form of neurofeedback might be as effective as long-term prescription medication, medical insurance coverage for treatment might prove a tough hurdle to clear. Still, she is keen on the possibilities that the technology offers. “It overcomes a lot of barriers to treatment for mental health, like taking a pill every day or talking to a stranger about your mother,” Young says. “The greatest challenge might be getting people to accept it as an intervention.”






More News
Daily briefing: Carrion crows have counting skills seen only in people
Researcher parents are paying a high price for conference travel — here’s how to fix it
Asymmetric hydrogenation of ketimines with minimally different alkyl groups – Nature