People lay flowers at a memorial for Junior Seau, a professional American football player who died of a self-inflicted gunshot wound in 2012.Credit: Sandy Huffaker/Getty
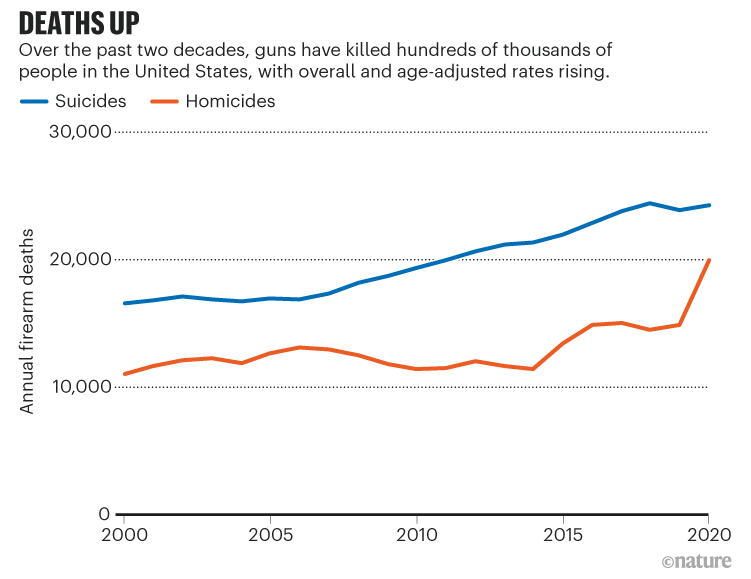
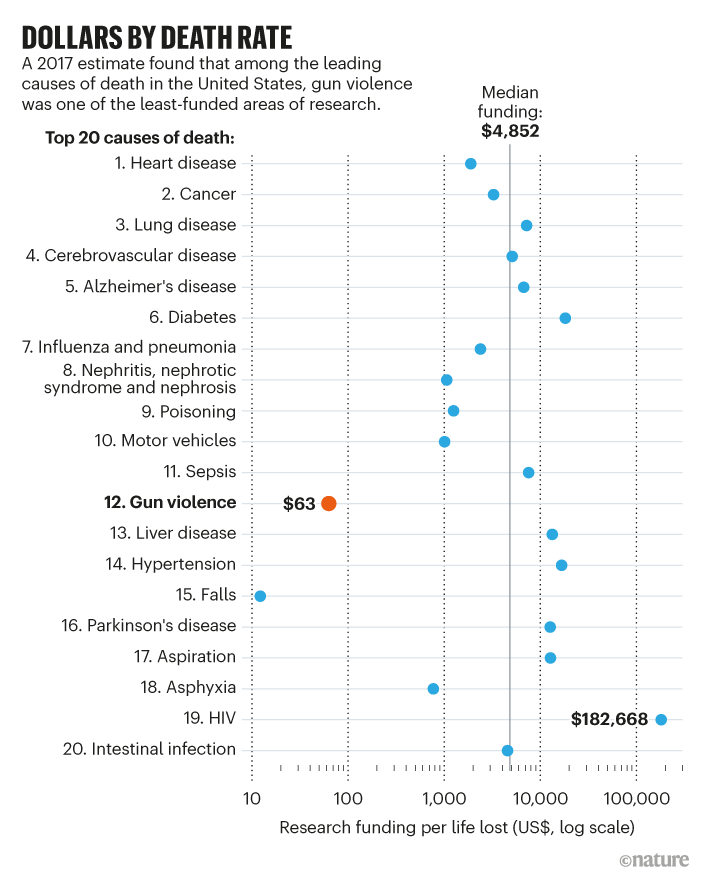
From 2001 to 2020, US cancer death rates fell by 27%. The nation’s traffic fatality rates per 100,000 people fell by about 21%, even counting a small rise in 2020. By contrast, US gun death rates went up: by 24% for suicide and by 48% for homicide1 (see ‘Deaths up’). In 2020, firearms became the leading cause of death for US children2. Yet firearm injury is among the least researched and worst funded of the leading causes of death in the United States3,4 (see ‘Dollars by death rate’).
We are clinicians, researchers and advocates who are convinced that more research on the topic can help to reduce deaths and injuries. It has helped in other fields. For instance, seatbelts in cars were initially considered an industry issue, but a public-health framing brought more data and encouraged effective safety measures. Better data and improved research have similarly informed comprehensive public-health strategies that have reduced issues from tobacco use and child drownings to lead poisoning and vaccine-preventable diseases. Providing evidence can inform strategies that both tackle the root causes of a problem and use timely, accurate data to iterate solutions. It will take more than data to reduce harm, but firm evidence and improved understanding can spur effective efforts.
According to a 2017 review, the volume of research publications related to firearm injury was only 4.5% of that predicted based on health burden4. A 2019 paper5 estimated that a 30-fold increase would be needed in funding for paediatric firearm-injury prevention alone to achieve funding levels on a par with other causes that have similar mortality rates. Despite recent improvements, the number of researchers in firearm-injury prevention remains low.
Source: CDC WISQARS database
The lack is largely due to two decades of firearm injury being treated more as a political topic than as a public-health problem. In 1996, Congress slashed the budget for firearm-injury prevention research at the Centers for Disease Control and Prevention (CDC) and passed legislation known as the Dickey Amendment, stating that CDC funds for injury prevention could not “be used to advocate or promote gun control”. In 2011, this language was extended to the US National Institutes of Health (NIH) and all agencies in the Department of Health and Human Services. Although not a formal prohibition, it effectively stymied research.
The tide is shifting. After a deadly shooting in 2018 at a school in Parkland, Florida, lawmakers clarified the policy and, in both 2020 and 2021, the US government approved a total of US$25 million in grants to the CDC and NIH for studying firearm injury. This level of funding is an improvement, but is still insufficient.
Firearm injury is a particular problem in the United States, and many leading US public-health and medical organizations have outlined consensus-based research agendas — including the American College of Surgeons, the American College of Emergency Physicians, the American Public Health Association and the National Academies of Sciences, Engineering, and Medicine. These feature rigorous data collection around preventive strategies to stem the growing numbers of firearm injuries and deaths, and call for firearm injury to be prioritized as a public-health discipline.
Public health follows a set approach: define and measure the scope of the problem; identify factors that raise or lower risk; design and evaluate interventions; and, finally, apply effective ones more broadly. The overarching strategy is to decrease harm by changing behaviour, altering environmental conditions (factors from health-care availability and traffic patterns to social networks) or reducing access to instruments of harm. For firearm injury, precise causes and prevention approaches will differ across communities and in intent (focusing on self-harm, unintentional injury or assault), but the need for evidence — and for researchers ready to collect it — applies broadly. Here, we describe how to fill those needs.
Source: RAND/Ref. 3/Nature
Collect comprehensive data
The main requirement in a public-health approach to firearm injury is to obtain data that are more accurate and more complete than those currently available6. A 2020 report7 by NORC, an independent research organization at the University of Chicago, Illinois, found the state of information woeful: “Data collection is haphazard and disorganized and it is of no surprise that our baseline understanding of the relationship between firearms and firearms injury and death are equally incomplete.”
It is clear that young Black men are much more likely to be injured or killed in an assault involving guns, and that middle-aged white, American Indian and Alaskan Native men are at the highest risk for suicide (from firearms, and generally). However, it is not enough merely to know that access to a firearm or membership of a broad demographic group increases risk1,2. Within a community or category, how do those injured by firearms differ from those who are not? Such data could identify risk and protective factors, help to assess what interventions can mitigate firearm injuries and determine the best way for programmes to be delivered.
US gun policies: what researchers know about their effectiveness
One of the most limiting data gaps is timely information on non-fatal firearm injuries. Many hospital-based sources of data misclassify the cause of firearm injuries, particularly because injuries of undetermined cause are classified as ‘unintentional’ by default, and determining the actual cause often requires an investigation by law-enforcement agencies. Delays and uncertainties mean that researchers cannot pinpoint locations and conditions where gun injury is more likely and where interventions might be introduced6.
Other gaps include the lack of data on whether the same person comes into a hospital with a gun injury more than once, what happens to them and whether they receive counselling about safe storage of the firearm or a referral to a violence-intervention programme. Nor is there any straightforward way to report the relationship between the shooter and those who are shot. Even states such as California that have been able to match firearm ownership and injury data for research purposes are losing access to these data because of new privacy rules.
Much could be improved, simply at the policy level. For example, questions about firearm injury could be included as part of ongoing national health surveys or data-collection efforts, such as the CDC’s Behavioral Risk Factor Surveillance System, its Youth Risk Behavior Surveillance System or the Nationwide Emergency Department Sample (run by the Agency for Healthcare Research and Quality). Revised national policies could make it easier to share data about patterns of firearm injury, and to make those data transparent for the public, as the city of Philadelphia in Pennsylvania is doing. Policy revisions could also remove restrictions that hinder researchers’ ability to identify hot spots of injury. One such restriction is the Tiahrt Amendment of 2003, which bars academics from accessing a database to trace guns used in crimes.
In its report7, NORC called for better harmonization of regional, state and local data; for researchers to have better access to existing information; and for data to be added on gunshot health outcomes, high-risk populations and social determinants of firearm use. Non-governmental sources of data, such as the non-profit Gun Violence Archive (www.gunviolencearchive.org), are emerging but still lack crucial information. Some combination of federal investment and philanthropy must fill these gaps. Otherwise, piecemeal and poorly collated data will impair even the best-funded science.
Learn to optimize interventions
Multiple groups, including the National Academies of Sciences, Engineering, and Medicine, have outlined the types of intervention that are likely to be effective in reducing firearm injury and death (see go.nature.com/3bnqj2t and go.nature.com/3svqdqw). These range from the individual to the societal level, and span disciplines. We cannot overemphasize the importance of ensuring that these interventions are effectively evaluated — both as they are initially developed and implemented, and over time. Doing this evaluation requires that the research community prioritizes the metrics that are most important to affected communities.
Miyoshia Bailey holds a photo of her son Cortez at a 2015 event calling for better gun control. He died after being shot in Chicago, Illinois.Credit: Allison Shelley/Getty
Researchers are working to develop and assess a variety of promising interventions. Community-based suicide-prevention programmes, for instance, can set up helplines for rural citizens and prompt people to talk to isolated, ageing parents about safe gun storage. School-based programmes could help students to identify mass-shooting threats. Hospital-based programmes might offer violently injured patients a suite of tailored support (such as housing, employment or legal services) and could train clinicians and violence-prevention professionals to counsel people about youth services, violence intervention and firearm storage, and provide gun locks8,9.
Gun violence is surging — researchers finally have the money to ask why
For all of these interventions, researchers and funders should invest in community partnerships10,11. In one example, a growing body of evidence suggests that certain individuals who are at high risk of firearm injury and violence are more open to discussions if they speak to someone with ‘lived experience’. Depending on the circumstances, that might be someone who has been incarcerated, survived a mass shooting, considered suicide, escaped domestic violence or experienced a family tragedy as a firearm owner (see, for instance, ref. 12). Regardless, all of these voices should be at the table when creating an intervention and planning its evaluation. This includes determining which data are gathered and from whom, and assessing whether a programme has succeeded.
Once an intervention has been shown to be effective, work should not stop. Strategies to implement firearm-injury prevention programmes remain largely uncharted8,9. Barriers include a lack of evidence on whether an intervention is effective, health-care providers’ worries about bringing gun-safety discussions into their practice, and insufficient funding to ensure that affected communities take part in designing research and interventions. Support for surmounting these barriers should be built into research infrastructure.
Catalyse collaborations
Everyone working in this field should be encouraged to reach outside their conventional area of focus10,11. For example, researchers at the non-profit health-care provider Northwell Health (where C.S. works) are collaborating with those investigating substance use to evaluate whether effective screening approaches in that field apply to gun safety8. The best public-health approaches synthesize inputs from disparate disciplines: engineers’ redesign of gun locks; sociologists’ measures of structural disparities and racism; urban planners’ introduction of green space; and insights from political scientists, economists, psychologists, legal scholars, data scientists and more.
Family members wait for news after a fatal school shooting in Parkland, Florida, in 2018.Credit: Wilfredo Lee/AP/Shutterstock
Community engagement is crucial, especially because gun advocates, members of affected communities and under-represented racial minority groups are often deeply sceptical of academic or government-funded researchers10. The Health Alliance for Violence Intervention, a non-profit group headed by F.L.D., organizes a national working group of violence-prevention researchers to integrate community participation into rigorous scientific studies. Funding agencies are increasingly open to supporting such community-based participatory research11. A growing number of researchers are including firearm owners or members of community organizations in their research teams and authorship lists, but more is needed: collaborations that extend beyond academia should not simply be enabled; they should be the default.
Build research cohorts and institutes
Reflecting the historical lapse in research, firearm injury is rarely integrated into public health or medical education. It is therefore often overlooked when graduate and medical students consider their specialisms. A 2020 survey13 of 244 medical residents in a New York City hospital found that only 14% felt confident discussing firearm safety with patients, and 66% said that their programmes did not offer training on the topic. Another 2020 study14 found that trainee paediatricians in Texas who attended a two-hour workshop session were five times more likely to discuss firearm safety with patients even six months after the workshop.
Fight the silencing of gun research
Organizations such as the National Collaborative on Gun Violence Research in Santa Monica, California (a network administered by the RAND Foundation to help philanthropists coordinate support for research), have supported some intrepid research since the Dickey Amendment. Alongside the federal funding in 2020 and 2021, some institutions have allocated internal funding and created endowments for research and education, but centres and hubs supporting the study of firearm injury are still sparse. We know of fewer than a dozen. This means that researchers in this field are disconnected, unable to share resources and limited in their ability to cross institutional boundaries.
Institutional homes for firearm-injury prevention — in a university, health-care system or city — can help to legitimize this work, catalyse inter-sectoral collaboration and speed the pace of knowledge generation. A bolus of research could help to counter widespread myths and untruths. An increase in the number and frequency of national forums focused on firearm injury, such as last month’s Medical Summit on Firearm Injury Prevention in Chicago and the National Research Conference on Firearm Injury Prevention in Washington DC at the end of November, is a sign of progress. Particularly helpful would be funds for pilot projects with community-based researchers, as well as seed funds and mentorship programmes to support researchers who are beginning their careers in the field.
Given the prevalence of firearm injury and death in the United States, it is astounding that scientific understanding of the problem is so poor and that the research infrastructure and workforce are so underdeveloped. As further funding emerges, it is crucial to build a field that honours the magnitude of the problem and builds up the collaborations and innovations necessary to save lives and create a more equitable society.
It has been immensely valuable to shift our national view of firearm-injury prevention away from a political issue and towards a public-health crisis. But that is only half the battle. For the public-health approach to make a difference to individuals, we have to engage communities, ask relevant questions and create and scale up the infrastructure necessary to obtain timely, actionable answers.












More News
Want to make a difference? Try working at an environmental non-profit organization
Bird flu virus has been spreading in US cows for months, RNA reveals
Judge dismisses superconductivity physicist’s lawsuit against university